
COVID-19 is forcing us to examine our immune health
As I stated in the previous article, very rarely are we put into a challenging situation that forces us to examine our immune health. Unless we get diagnosed with an unusual immune disorder, most of us don’t give much thought to our immune system and what it requires to protect us from pathogens we are exposed to on a daily basis. SARS-COV2 (the coronavirus that causes COVID-19) is forcing us to take a closer look at our immune health and whether it is well-suited to defend against this novel coronavirus. Unfortunately, beyond avoiding potential exposures through social distancing, the use of face masks and sanitizer, most of us don’t give much thought to how our immune system is fighting diligently to protect us from constant bacterial and viral threats. But how do we develop a strong immune system and what do we need to do to maintain it? What makes one person’s immune system able to defend against COVID-19 while another’s cannot rise up to the challenge? This article examines the requirements of a strong and effective immune system.
The immune system needs to be trained effectively
There are certain things that are important to our immune development that have already been predetermined before we have a say in the matter. We all know that breastfeeding is important to impart major protective components to the infant, including secretory IgA (SIgA) antibodies and lactoferrin. We have all heard that the breastfed infant is better protected against numerous common infections than non-breastfed infants (1). And we all know that natural vaginal childbirth allows the fetus to be exposed to beneficial bacteria through the vaginal canal that play an important role in the development of the fetal immune system (2). But did you know that compared with vaginal delivery, CS delivery is associated with increased risks of a multitude of immune disorders later in life, such as asthma, allergies, autoimmune disorders such as type 1 diabetes, celiac disease and inflammatory bowel diseases, immune deficiencies, and childhood cancers such as leukemia and other malignancies (3)? Did you know that our immune system starts developing in utero shortly after our brain and continues developing after birth and is affected by a number of environmental factors both in the womb and after birth? Studies show that environmental insults during pregnancy, such as infection or malnutrition, seem to dramatically impact brain development (4).
 The Thymus as Boot Camp for the Soldiers of the Immune System
The Thymus as Boot Camp for the Soldiers of the Immune System
Throughout childhood and puberty, the thymus (critical organ of the developing immune system) serves a vital role in the training and development of T-lymphocytes (or T cells), an extremely important type of white blood cell. T cells, part of the adaptive immune system, defend the body from potentially deadly pathogens such as bacteria, viruses, and fungi. The thymus receives immature T cells from the bone marrow and trains them to attack foreign cells and viruses. The T cells that attack foreign cells and viruses appropriately are selected to survive (positive selection) while the T cells that bind to the body’s own antigens leading to autoimmunity are eliminated (negative selection) (5). In this way, the immune system is effectively trained to differentiate foreign antigen (ie: bacteria, viruses, fungi) from self-antigen (the body’s own tissue).

The immune system needs to be strong enough to defend against potential threats
There are about 1400 species of human pathogens (disease-causing organisms) that have been identified, including various bacteria, mycobacteria, archaea, viruses, fungi, parasites such as protozoans, worms, and prions. Some of these pathogens are responsible for some of the most deadly diseases the world has ever seen, such as the Black Plague, Spanish Flu, malaria, AIDS, tuberculosis, measles, influenza and now the novel SARS-CoV2 coronavirus. The new species of human pathogenic threats that are emerging are primarily viruses and are mostly associated with animal reservoirs (6). A healthy, robust and resilient immune system will be able to cope with most of the pathogenic challenges it will face during its lifetime. However, a weakened or compromised immune system may not be able to defend against many of these challenges it will face.
The immune system needs to be smart enough to avoid autoimmunity
One common immune disorder we are seeing more and more frequently is autoimmune disease. According to the National Institutes of Health, up to 23.5 million Americans (more than seven percent of the population) suffer from an autoimmune disease—and the prevalence is rising (7). Autoimmunity occurs when the immune system loses the ability to differentiate self-antigen (protein) from foreign antigen (ie: pathogen protein), one of the hallmarks of the healthy immune system, and starts attacking the body. In autoimmunity, the body’s own defense system becomes so dysregulated that it initiates immune (inflammatory) responses against the tissue it is designed to protect. Once this occurs, there is no going back, as the immune system is now primed to continue these attacks indefinitely. The immune system can become overzealous at times and upregulate these attacks on the person’s tissues and organs when internal or external factors trigger these flare-ups and sometimes multiple tissues simultaneously. Not surprisingly, when it comes across a pathogen that poses a threat, it may not be able to defend against it very efficiently because its resources are being spent in other ways. To make matters worse, many of these autoimmune individuals are on medication to suppress their immune system, making them very vulnerable to new pathogens, such as viruses.
 Importance of Metabolic Health
Importance of Metabolic Health
In the last article, we discussed the science showing those with poor metabolic health have a much harder time defending against this virus. Why is that? Because these metabolic disorders are mediated by chronic inflammation which causes dysregulation to the immune system and makes it less efficient at responding to viral threats. One group of researchers on this topic describes the cross-talk between the immune and metabolic systems as “pivotal in promoting ‘metabolic health’ throughout the life of an organism” and plays a fundamental role “in its adaptation to ever-changing environmental makeups and nutritional availability” (8). In other words, the constant communication that occurs between the immune and metabolic systems enable the person to to adapt to changes in their diet and environment. These researchers go on to say “perturbations in this intricate immune-metabolic cross-talk contribute to the tendency to develop altered metabolic states that may culminate in metabolic disorders such as malnutrition, obesity, type 2 diabetes mellitus (T2DM), and other features of the metabolic syndrome”. Basically, it is the breakdown of this communication between the immune and metabolic systems that leads to these chronic metabolic diseases. According to these researchers, key regulators of these immune-metabolic interactions include host genetics, nutritional status, and the intestinal microbiome (8).
Importance of Gut Health
The gut plays many roles in supporting overall immune health and our gut bacteria (microbiome) lie at the center of these functions. First, our microbiome functions to defend against harmful organisms, helps train the gut immune system to identify friend or foe (yes, the gut has its own immune system) and helps degrade toxic compounds. It also is able to digest certain foods that are not digestible by the human GI tract (ie: fiber such as cellulose) and produce compounds (ie: short chain fatty acids) that help the gut immune system react appropriately to antigens (proteins) and help protect against cancers. The gut bacteria also facilitate the absorption of dietary minerals (ie: magnesium, calcium and iron) and synthesize some essential vitamins (ie: vitamin K and folate) and amino acids (the building blocks of proteins).
 Usually, we coexist ‘peacefully’ with our commensal microflora (mutualism), which has been established through evolution on both sides. The bacteria benefit from the stable habitat, which is rich in energy sources from the food we ingest and the host benefits from these bacteria in these numerous ways described above (9). However, the intestinal flora are affected by several factors, such as diet, climate changes, stress, illness, aging and medications, such as acid-suppressing and antibiotic medications (10).
Usually, we coexist ‘peacefully’ with our commensal microflora (mutualism), which has been established through evolution on both sides. The bacteria benefit from the stable habitat, which is rich in energy sources from the food we ingest and the host benefits from these bacteria in these numerous ways described above (9). However, the intestinal flora are affected by several factors, such as diet, climate changes, stress, illness, aging and medications, such as acid-suppressing and antibiotic medications (10).
The gut lining also plays a critical role in immune health, acting as a barrier to the body, protecting it from the toxic compounds found in the gut. Toxins in the gut, including endotoxins from gut bacteria, environmental toxins and pathogens, need to be prevented from entering blood circulation. The gut bacteria play an important role in supporting this barrier function by binding to epithelial cells and inhibiting pathogen binding, enhancing barrier function (11). Any compromise to this gut barrier allows toxins into circulation causing immune disruption and increased workload on the organs of toxification, particularly the liver. Intestinal permeability or ‘leaky gut’ is a very common cause of inflammation in the body and can result from many different types of scenarios, including poor diet, chronic stress, poor sleep, hormone imbalances, blood sugar imbalances and medications. This is probably the most common condition that I see in the clinic that causes major inflammation in the body and is likely the predominant breakdown that leads to autoimmunity, according to the most recent research (12, 13). For more on this topic, you can read this article.
 Diet and Nutrition
Diet and Nutrition
Nutrition is a critical part of the immune response and malnutrition is the most common cause of compromised immune health worldwide (14). Undernutrition is well understood to impair immune function and the extent of impairment that results will depend upon the severity of the deficiency, the presence of infection and the person’s age (15). The cells and organs of your immune system, like any other cells and organs of the body, require a variety of macro and micronutrients to function optimally, including a broad range of amino acids, vitamins, minerals, antioxidants and nutrients that support antioxidant enzymes, white blood cells and various immune responses. All antibodies (immunoglobulins), which are critical in cell-mediated immunity, are made of proteins, as is the complement system, secretory IgA and cytokines (inflammatory mediators). Micronutrients such as zinc, selenium, iron, copper, vitamins A, C, D, E, and B vitamins have important influences on immune responses. Some of the key micronutrients for immune function are discussed below in Immune Supporting Nutrients and Herbs.
What you put into your mouth eventually is digested into nutrients that either serve a useful purpose in immune health (ie: source of fuel for immune reactions, provide direct or indirect support to immune pathways or immune mediator proteins, or protect the body against toxins and oxidative stress) or cause damage to the body leading to inflammation (ie: toxins, advanced glycated end-products or AGEs, reactive oxygen species, etc.). Remember, inflammation is your body’s response to any tissue damage, toxicity or pathogenic entry.
Another way to look at any given food is it either promotes inflammatory or anti-inflammatory responses. The foods that have the latter effect are the foods that are recommended in the anti-inflammatory diets used in the naturopathic and functional medicine circles. These tend to be whole, high-fiber diets, high in fruit, vegetables, plant-based proteins, fish, legumes, nuts, and seeds and healthy fats. Meats can also be part of an anti-inflammatory diet if they are grass-fed and free of hormones and antibiotics. The Mediterranean diet and Paleo diet are examples of these. While some people can handle grains, others can’t and this can be a source of inflammation in these people, particularly in the autoimmune population. Chronic inflammation, as you recall, leads to immune dysregulation and sets you up for failure against viral challenges that require a healthy, robust response from the immune system.
 Adequate Sleep and Rest
Adequate Sleep and Rest
Sleep has long been known to play a critical role in immune health. Sleep affects various aspects of immune function and is associated with reduced risk of infection, and has been demonstrated to improve recovery from infections and vaccination responses (16). Prolonged sleep deficiency (ie: short sleep duration, sleep disturbance) can lead to chronic, systemic low-grade inflammation and is associated with diabetes, atherosclerosis, and neurodegeneration, which are all driven by inflammation (17). In a recent study, scientists demonstrated that quality sleep bolsters the function of T cells in your body that fight off viral infection. Good sleep does this by enhancing the ability of T cells to adhere to and destroy cells infected by viruses and other pathogens (18).
The sleep-wake cycle and the 24-hour circadian rhythm of adrenal hormones such as cortisol also exerts a strong regulatory influence on immune function. Just like adrenal hormones have a circadian rhythm, recent research demonstrates our immune system also has a circadian rhythm. Certain white blood cells (ie: naïve T cells) and inflammatory cytokines peak during early sleeping hours while others (ie: cytotoxic NK cells) and anti-inflammatory cytokines peak during the day (19). Sleep also appears to play another role in improving the formation of immunological memory T helper cells and antibody production, allowing your immune system to defend more efficiently against future infection (20).
 Stress Management
Stress Management
Ever since the pioneering research performed by Hans Selye in the 1930’s, we have known that chronic stress has profound impacts on the immune system. Chronic stress is now well-known to suppress immune function and increase susceptibility to infections and cancer while acute stress is known to exacerbate asthma, and allergic, autoimmune and inflammatory diseases, most likely by causing immune dysregulation (21). Chronic or long-term stress can suppress immune function by decreasing immune cell count and function and increasing immunosuppressive mechanisms (22). Chronic stressors are associated with decreased cytotoxic T-cell and natural killer (NK) cell activity which are critical in fighting viral infection (23). Chronic stress can also dysregulate immune function by promoting proinflammatory and Th-2 cytokine-driven responses (24).
Numerous studies have shown the benefits of relaxation and stress management techniques such as guided imagery, mindfulness meditation, breathing exercises and tai-chi in improving immune health. Social connections have been associated with a strong immune system. Even positive emotions such as happiness can have positive effects on immune health (25-29).
 Avoidance of Toxins
Avoidance of Toxins
We are living in a world that has changed dramatically just within our lifetimes. We are now exposed to countless chemicals, hybridized foods, genetically-modified foods, all of which are very immune-activating. There are now more than 84,000 different chemicals used in making products such as food, clothes, furniture, electronics and toys that we are potentially exposed to on a daily basis and about 1,500 new chemicals are introduced each year (30). Environmental chemicals are linked with various cancers, obesity, diabetes, heart disease, brain degeneration, neurological disorders and almost every known health issue, largely due to immune dysregulation and the chronic inflammation that develops (31). These links can be difficult to identify and the published data difficult for the average person to understand. Unless there is an acute exposure, exposure to chemical pollutants usually occurs gradually over a long period of time and effects tend to be cumulative in the body. This contributes to what is known as the individual’s ‘toxic burden’, which we pay close attention to in functional medicine.
 However, environmental toxins are not the only toxins we are exposed to unfortunately. There are also toxins generated endogenously (from within our bodies) that are produced by an imbalanced microbiome, such as lipopolysaccharides (endotoxins) that can enter circulation in conditions of intestinal permeability (leaky gut) and wreak havoc on our immune health. In addition to bacterial overgrowths, yeast or fungal overgrowth or other hidden infections can produce endotoxins which can also wreak havoc on our immune systems. Additionally, excess production of hormones (or decreased capacity to metabolize and clear these hormones by our detoxifying organs) can also lead to inflammation and immune dysregulation and decrease our capacity to clear other toxins. Therefore, in order to have a healthy immune system, we must be active in avoiding unnecessary environmental toxins on a daily basis, support gut health, prevent and treat any pathogenic overgrowths or infection, maintain hormonal balance and support hepatic (liver) detoxification.
However, environmental toxins are not the only toxins we are exposed to unfortunately. There are also toxins generated endogenously (from within our bodies) that are produced by an imbalanced microbiome, such as lipopolysaccharides (endotoxins) that can enter circulation in conditions of intestinal permeability (leaky gut) and wreak havoc on our immune health. In addition to bacterial overgrowths, yeast or fungal overgrowth or other hidden infections can produce endotoxins which can also wreak havoc on our immune systems. Additionally, excess production of hormones (or decreased capacity to metabolize and clear these hormones by our detoxifying organs) can also lead to inflammation and immune dysregulation and decrease our capacity to clear other toxins. Therefore, in order to have a healthy immune system, we must be active in avoiding unnecessary environmental toxins on a daily basis, support gut health, prevent and treat any pathogenic overgrowths or infection, maintain hormonal balance and support hepatic (liver) detoxification.
 Immune-Supporting Nutrients and Herbs
Immune-Supporting Nutrients and Herbs
The immune system, like any other system in the body, requires a wide variety of vitamins, minerals and other nutrients to function optimally. Based on available studies, Vitamin A, vitamin C, vitamin D, N-acetylcysteine or glutathione, zinc, selenium, and essential fatty acids appear to be some of the most important nutrients to maintain immune health and fight viral infection (32). In addition, there are a number of herbs such as licorice root, echinacea, astragalus, elderberry, olive leaf, oregano oil and berberine that have been shown to have antiviral effects by either preventing viral binding to cells, blocking viral replication or having direct antiviral effects. In addition, many herbs have been shown to improve immune responses against viruses, by exhibiting antioxidant or anti-inflammatory effects or promoting cell function in other ways. Here is a list of those nutrients and herbs and the key roles they play to defend against viral infection.
 Vitamin A
Vitamin A
- Efficacy against a wide-range of bacterial and viral infections (33, 34)
- Essential for normal immune function, growth, development and maintenance of epithelial cells (GI tract)
- Subclinical deficiency results in increased susceptibility to common infectious disease (WHO)
Vitamin C
- Potent antiviral agent (35, 36, 37)
- Important antioxidant and immune stimulant
- Shortens duration and severity of symptoms of the flu and common cold (38, 39)
- Breaks down histamine and so has anti-histamine function
- IV vitamin C used to successfully treat COVID-19 patients in China (40)
 Vitamin D
Vitamin D
- Enhances vitamin A function (41)
- Improves gut barrier function (42)
- Enhances both specific and non-specific innate immunity in a wide range of viral infections including HIV, HPV, hepatitis (43-46)
- Reduces systemic inflammation, neuroinflammation
- Improves mitochondrial function and muscle strength
Zinc
- Reduces severity and duration of common cold symptoms (47)
- Inhibits viral replication by blocking RNA polymerase activity
- Reduces mortality for a wide range of infectious diseases
- Provides antioxidant benefits
- Important for gut barrier function
 Selenium
Selenium
- Functions to reduce viral replication and viral mutation (48)
- Provides anti-inflammatory and antioxidant effects
- Increases glutathione (GSH) levels
N-Acetyl-Cysteine (NAC)
- Direct and indirect antioxidant (49)
- Increases production of glutathione (GSH)
- Supports phase II conjugation and protects the liver
- Anti-inflammatory and inhibits replication of influenza A (50)
- Improves cell-mediated immunity (51)
- Mucolytic
- Disrupts biofilms
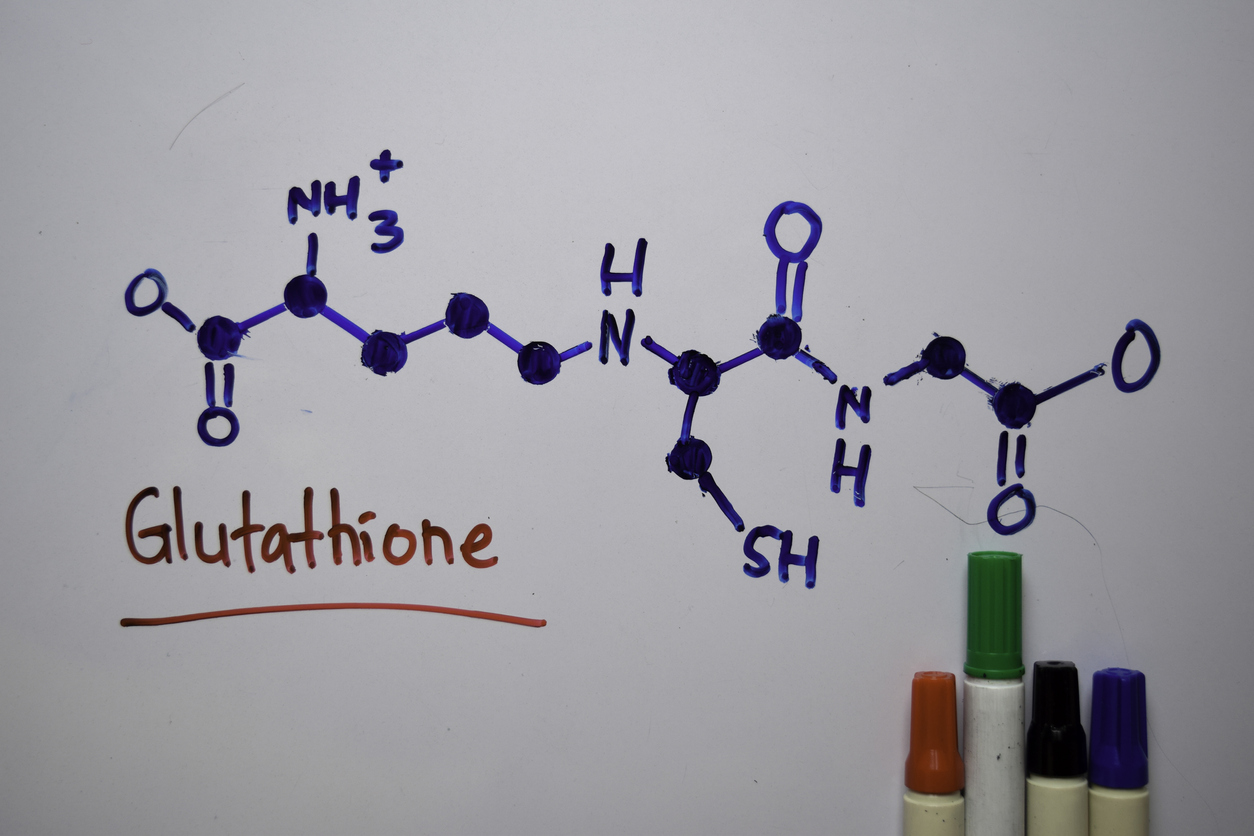 Glutathione (GSH)
Glutathione (GSH)
- Critical intracellular antioxidant
- Regulates both innate and adaptive immune responses
- Regulates NK cell activity
- Helps balance Th1 and Th2 activity
Colloidal Silver
- Shown to be effective against a wide variety of viruses, including HIV, HBV, HSV, RSV and monkey pox virus (52)
- Shown to reduce and prevent infection from HSV and the parainfluenza type 3 virus (53)
- Significantly protected cells from H3N2 flu infection and prevented viral growth in the lungs
- Shown to inhibit flu virus’ binding capacity to a cell’s membrane

Licorice Root (Glycyrrhiza glabra)
- Used to treat respiratory tract infections for thousands of years in China (54)
- Shows activity against a wide variety of RNA and DNA viruses
- Used intravenously to treat chronic hepatitis B and C infections
- Directly inhibits replication of SARS-associated coronavirus and inhibits binding and penetration of the virus (55, 56)
- 2003 Lancet article recommended assessing for treatment of SARS (57)
Astragalus (Astragalus membranaceus)
- Used to treat respiratory infections for thousands of years in China
- Found to inhibit influenza proliferation
- Exhibits antiviral properties against infectious bronchitis caused by avian (bird) coronavirus and avian influenza (58, 59)
- Exhibits anti-inflammatory and antioxidant effects (60, 61)
 Elderberry (Sambucus nigra)
Elderberry (Sambucus nigra)
- Shortens the length of influenza infection by 4 days (62)
- Effective in vitro against 10 different influenza strains (63)
- Inhibits the flu virus’s entry and replication in human cells
- Inhibits coronavirus activity at the point of infection (64)
- Can inhibit viral uptake and viral budding (preventing infection) (65)
Echinacea (Echinacea purpurea)
- Has multiple immune-modulatory and broad antiviral effects (66, 67)
- Prevents influenza A, avian flu, and swine flu and has activity against herpes simplex 1 and 2 in vitro
- Kills HIV-1
- Shows antiviral activity to several strains of influenza viruses, herpes simplex virus, respiratory syncytial virus, and rhinoviruses (68, 69)
- Modifies the clinical course of flu-like respiratory infection (70)
- Shown to decrease frequency of common cold
 Olive Leaf (Olea europaea)
Olive Leaf (Olea europaea)
- Inhibits numerous viruses in vitro , including parainfluenza, herpes, pseudorabies, and some forms of polio
- Shown to have antiviral effects against enveloped viruses
- Inhibits replication of HIV (71)
- Inhibits viral assembly at the cell membrane, stopping viral shedding (72)
- Six antiviral agents in olives identified to be effective against parainfluenza (73)
Oregano Oil (Origanum vulgare)
- Shown to have broad-range antibacterial and antiviral effects (74, 75)
- Shown partial efficacy against respiratory syncytial virus, coxsackie virus B3, and HSV1 (76)
- Effective against acute otitis media caused by H. influenzae (77)
- Inhibits virus’ ability to translate proteins for viral binding to cells
 Berberine
Berberine
- Decreases production of inflammatory cytokines such as TNF-alpha and IL-6 (78)
- Reduces inflammation through inhibition of various inflammatory pathways (79)
- Acts as a protease inhibitor for HIV (80)
- Reduces viral replication of respiratory syncytial virus (RSV) and reduces IL-6 mRNA (81)
Key Takeaways to Promote a Healthy Immune System
- Optimize metabolic health and exercise regularly
- Optimize gut health, including intestinal barrier function and gut flora balance
- Adopt a plant-based diet rich in fruits and vegetables and fish and seafood, avoiding processed meat and all processed foods
- Ensure adequate sleep and exercise
- Manage stress with stress-reduction activities (breathing, meditation, etc.)
- Avoid environmental toxins, cigarettes and heavy metals (including dental amalgams)
- Optimize intake of immune-support nutrients (vitamins A, C, E, zinc, selenium, NAC, etc.)
- Consider antiviral herbs for prevention or management of viral infection (consult with herbalist for best results)
References
- https://www.ncbi.nlm.nih.gov/pubmed/12727640
- https://www.sciencedaily.com/releases/2018/11/181130094328.htm
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5599043/
- https://www.hindawi.com/journals/np/2016/3597209/
- https://www.innerbody.com/image_endoov/lymp04-new.html
- https://www.tandfonline.com/doi/full/10.1080/10408410701647560
- https://www.niaid.nih.gov/sites/default/files/adccfinal.pdf
- https://www.sciencedirect.com/science/article/pii/S1550413117300967
- https://www.nature.com/articles/nri1373?cacheBust=1508280662071
- https://www.ncbi.nlm.nih.gov/pubmed/22366773
- https://onlinelibrary.wiley.com/doi/full/10.1111/j.1365-2036.2008.03750.x
- https://www.ncbi.nlm.nih.gov/pubmed/16265432
- https://www.ncbi.nlm.nih.gov/pubmed/19538307
- https://www.ncbi.nlm.nih.gov/pubmed/9250133
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6723551/
- https://journals.physiology.org/doi/full/10.1152/physrev.00010.2018
- https://journals.physiology.org/doi/full/10.1152/physrev.00010.2018
- https://rupress.org/jem/article/216/3/517/120367/G-s-coupled-receptor-signaling-and-sleep-regulate
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3256323/
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3256323/
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2790771/
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2790771/
- https://www.sciencedirect.com/science/article/abs/pii/S1470204504015979
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2790771/
- https://www.karger.com/Article/Abstract/288872
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4940234/
- https://journals.sagepub.com/doi/abs/10.4278/ajhp.081013-LIT-248
- https://www.nature.com/articles/nn.3086
- https://www.sciencedirect.com/science/article/abs/pii/S1568997206000279
- https://pubmed.ncbi.nlm.nih.gov/23027564/
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6356139/
- https://www.ncbi.nlm.nih.gov/pubmed/11781377
- https://www.ncbi.nlm.nih.gov/pubmed/11375434
- https://jlb.onlinelibrary.wiley.com/doi/10.1189/jlb.71.1.16
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7110025/
- https://www.ncbi.nlm.nih.gov/pubmed/9306475
- https://www.ncbi.nlm.nih.gov/pubmed/23700397
- https://www.ncbi.nlm.nih.gov/pubmed/7814237
- https://www.ncbi.nlm.nih.gov/pubmed/10543583
- https://clinicaltrials.gov/ct2/show/NCT04264533
- https://jlb.onlinelibrary.wiley.com/doi/10.1189/jlb.71.1.16
- https://www.ncbi.nlm.nih.gov/pubmed/22647055
- https://news.harvard.edu/gazette/story/2017/02/study-confirms-vitamin-d-protects-against-cold-and-flu/
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3166406/
- https://doi-org.uws.idm.oclc.org/10.1016/j.gene.2018.08.017
- https://doi-org.uws.idm.oclc.org/10.1016/j.jcv.2010.12.006
- https://jlb.onlinelibrary.wiley.com/doi/10.1189/jlb.71.1.16
- https://jlb.onlinelibrary.wiley.com/doi/10.1189/jlb.71.1.16
- https://jlb.onlinelibrary.wiley.com/doi/10.1189/jlb.71.1.16
- https://www.ncbi.nlm.nih.gov/pubmed/19732754
- https://www.ncbi.nlm.nih.gov/pubmed/9230243
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6264685/
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3826769/
- https://www.researchgate.net/publicahttps://onlinelibrary.wiley.com/doi/10.1002/jmv.25707tion/261442961_Prevention_and_treatment_of_viral_respiratory_infections_by_traditional_Chinese_herbs
- https://www.ncbi.nlm.nih.gov/pubmed/15715493
- https://www.ncbi.nlm.nih.gov/pubmed/15885816
- https://www.nature.com/articles/news030609-16
- https://www.ncbi.nlm.nih.gov/pubmed/29170045
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3729712/
- https://www.ncbi.nlm.nih.gov/pubmed/30586589
- https://www.ncbi.nlm.nih.gov/pubmed/32057253
- https://www.ncbi.nlm.nih.gov/pubmed/15080016
- https://www.ncbi.nlm.nih.gov/pubmed/9395631
- https://www.ncbi.nlm.nih.gov/pubmed/31560964
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5610768/
- https://www.ncbi.nlm.nih.gov/pubmed/26009695
- https://www.ncbi.nlm.nih.gov/pubmed/22131823
- https://www.ncbi.nlm.nih.gov/pubmed/22131823
- https://www.reliasmedia.com/articles/11276-echinacea-for-upper-respiratory-viral-infections-preparatory-differences-matter
- https://www.reliasmedia.com/articles/11276-echinacea-for-upper-respiratory-viral-infections-preparatory-differences-matter
- https://www.ncbi.nlm.nih.gov/pubmed/12878215
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2790717/
- https://www.ncbi.nlm.nih.gov/pubmed/11724241
- https://www.ncbi.nlm.nih.gov/pubmed/29744941
- https://www.ncbi.nlm.nih.gov/pubmed/24779581
- https://www.sciencedirect.com/science/article/abs/pii/S0308814613018438
- https://www.ncbi.nlm.nih.gov/pubmed/15871121
- https://www.ncbi.nlm.nih.gov/pubmed/20161729
- https://www.ncbi.nlm.nih.gov/pubmed/30306659
- https://www.ncbi.nlm.nih.gov/pubmed/20161729
- https://www.ncbi.nlm.nih.gov/pubmed/25939536