Hashimoto’s disease is a condition in which the immune system attacks the thyroid leading to hypothyroidism.
Hypothyroidism (underactive thyroid) is a condition in which the thyroid gland doesn’t produce enough thyroid hormones which regulate metabolic rate.
Hashimoto’s disease is the most common cause of hypothyroidism in the United States and may account for up to 90% of hypothyroid cases. It primarily affects women but also can occur in men and in children.

Lab assessment of hypothyroid patients should include thyroid antibodies, to assess for autoimmune thyroid conditions.
If thyroid antibodies are positive, additional testing may include intestinal permeability lab testing (to assess for leaky gut), stool testing (to rule out an imbalance of gut bacteria) and food sensitivity testing.
There are 4 areas of management of autoimmune conditions in the Functional Medicine approach:
Lab testing is a critical first step in identifying the extent of systemic inflammation and ruling out many environmental insults which act as triggers and mediators of autoimmunity, such as chronic infection, heavy metal toxicity and decreased capacity to perform liver detoxification. Food sensitivities can also promote inflammation and potentially drive autoimmune responses. Identifying and addressing these issues is critical in autoimmune patients to minimize damage and promote restorative function.
Functional Medicine addresses diet and lifestyle issues as well as using anti-inflammatory and immune-modulating herbs and nutritional compounds to decrease immune responses to self-tissue. Identifying the triggers of autoimmunity and modulating the immune response can have powerful long-term positive effects on slowing or stopping tissue destruction and improving quality of life.
There are a number of natural compounds that help support a faster recovery by breaking down offending triggers, increasing blood flow to target tissue, and dampening the immune response.
 Addressing Associated Conditions and Promote Autoimmune Responses
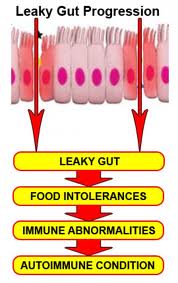
Addressing Associated Conditions and Promote Autoimmune ResponsesThere is growing evidence that increased intestinal permeability plays a pathogenic role in various autoimmune diseases. Increased intestinal permeability and compromised gut integrity appears to precede AI disease and predisposes to immune activation and chronic inflammation. Assessment and proper restoration of the integrity of the intestinal barrier is crucial in managing autoimmune conditions. Read More on Leaky Gut
There is growing evidence that increased intestinal permeability plays a pathogenic role in various autoimmune diseases. Identifying the existence of intestinal permeability and addressing this condition, leads to a more comprehensive and satisfactory outcome in the autoimmune patient.
Some foods can provoke immune responses and promote attacks against the thyroid, including gluten (found in wheat), corn, soy and dairy. Food sensitivity testing helps to identify and avoid these foods.
Milpitas: 408-262-6606
1649 S. Main Street, Ste. 102
Milpitas, CA 95035
Oakland: 510-350-8082
6232 La Salle Ave
Oakland, CA 94611