 In parts 4, 5 and 6 of this series, we examine the connection between gluten sensitivity, leaky gut and autoimmune disease. In this article, we focus on gluten sensitivity. What is gluten sensitivity and how is it different from celiac disease? What are the most common symptoms and signs associated with non-celiac gluten sensitivity? How common is it? Why are we seeing such an increase in this condition? How can I find out if I am sensitive to gluten?
In parts 4, 5 and 6 of this series, we examine the connection between gluten sensitivity, leaky gut and autoimmune disease. In this article, we focus on gluten sensitivity. What is gluten sensitivity and how is it different from celiac disease? What are the most common symptoms and signs associated with non-celiac gluten sensitivity? How common is it? Why are we seeing such an increase in this condition? How can I find out if I am sensitive to gluten?
 Gluten Sensitivity
Gluten Sensitivity
Without question, there has been an explosion of three major factors of chronic inflammation which leads to many chronic diseases: gluten sensitivity, intestinal permeability and autoimmune disease. It appears that these three factors combine to create vicious cycles leading to various ailments and symptoms. For example, gluten sensitivity leads to leaky gut and leaky gut leads to gluten sensitivity. Both gluten sensitivity and leaky gut have been shown to be major contributors to various autoimmune responses. Also, the inflammatory response of autoimmunity promotes tight junction breakdown and intestinal permeability and gluten sensitivity. We don’t know where it may start in any individual. But we do know that any of these can increase the risk of developing any other. (1) In this article, we explore the important topic of gluten sensitivity.
 What’s all the fuss about gluten sensitivity?
What’s all the fuss about gluten sensitivity?
Gluten sensitivity is defined as an immune response to gluten; it is not to be confused with an allergy. By strict definition, an allergy is a clear IgE-mediated response to an offender and may create anaphylaxis (a severe allergic reaction to an allergen). Gluten sensitivity is a IgA, IgM or IgG-mediated response to gluten and is not typically involved in anaphylaxis. This is important, because the gluten sensitivity response will not be identified with conventional allergy tests that use skin testing or IgE responses. Gluten sensitivity promotes an immune response that increases systemic inflammation and has been associated with a multitude of health conditions in the peer-reviewed literature. (2)
 What’s the difference between gluten sensitivity and celiac disease?
What’s the difference between gluten sensitivity and celiac disease?
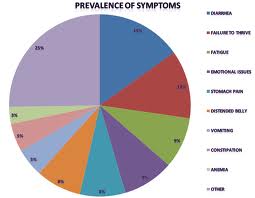
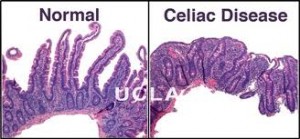
Celiac disease is a relatively rare (yet increasingly common) severe intolerance to gluten in which the immune system attacks and destroys the gastrointestinal tract on exposure to gluten. It affects approximately 1 in 100 people, or about 3 million Americans, most of whom are not diagnosed. (3) It can create a diverse range of gastrointestinal symptoms, such as bloating, gas, abdominal pain and cramping and diarrhea and may be associated with other symptoms including anemia, depression, joint pain, muscle pain, skin rashes and numbness and tingling anywhere in the body. This is diagnosed through conventional blood tests and may require intestinal biopsy. However, gluten sensitivity, which is much more common, has been associated with most of these symptoms, but others as well, including migraines, ADD/ADHD, autism, neurodegenerative disease, such as Alzheimer’s and Parkinson’s disease, autoimmune thyroid/hypothyroidism, autoimmune hepatitis, fibromyalgia, obesity and various skin problems. (4) This condition is much more difficult to diagnose because conventional lab testing is not reliable to assess risk of gluten sensitivity. Specialized testing (or a gluten-free diet) is required to assess this condition, which we will discuss later. This is why it is so underdiagnosed by doctors and other healthcare providers. Let’s first look at how celiac disease was first identified and how it is currently diagnosed.
 How is celiac disease diagnosed?
How is celiac disease diagnosed?
Celiac disease was first identified in 1950 by a Dutch pediatrician, Willem-Karel Dicke. In the 1960’s, gastroenterologists further studied the disease and were able to identify characteristic destruction patterns with celiac disease by studying intestinal tissue biopsies. This research has found two genotypes associated with increased risk of celiac disease: HLA-DQ2 and HLA-DQ8. Most celiac patients have the variant HLA-DQ2 allele. Researchers also found that celiac disease has specific antibodies that could be measured in the blood, such as gluten antibodies and transglutaminase antibodies. Over time, different criteria have been developed to diagnose celiac disease. Initially, celiac disease was thought to be a gastrointestinal disorder that was only a problem for susceptible people with certain genes who ingested gluten, leading to the destruction of the intestinal tract. This initial concept has now been challenged by research studies.
 Gluten sensitivity affects much more than just the intestinal tract!
Gluten sensitivity affects much more than just the intestinal tract!
Many people who have gluten sensitivity do not have intestinal manifestations. Instead, it can affect other tissues, such as the brain, peripheral nerves, thyroid, joints, etc. These are referred to as extraintestinal manifestations. The most common system affected by gluten is the nervous system. In fact, one study found that patients with intestinal complaints represent only a third of patients with neurological manifestations and gluten sensitivity!
“Patients with an enteropathy (disease of the intestinal tract) represent only a third of patients with neurological manifestations and gluten sensitivity.”(5)
In a study of 10 subjects who had headaches, walking abnormalities and elevated antigliadin antibodies, seven demonstrated complete resolution of symptoms with a gluten-free diet. The most interesting part of the study was that 6 out of the 10 subjects had no intestinal complaints! (6)
 Gluten sensitivity commonly causes neurological problems
Gluten sensitivity commonly causes neurological problems
Gluten sensitivity may manifest in a number of neurological deficits, depending on what part of the brain or nervous system is affected, including numbness and tingling in any part of the body (peripheral neuropathy), balance problems (ataxia), migraines, attention-deficit problems or ADHD, “brain fog”, and cognitive deficits. (7, 8, 9)
A recent paper entitled, “The Gluten Syndrome: a neurological disease” reported findings that gluten sensitivity that is unassociated with celiac disease or gastrointestinal destruction can cause harm to the brain and nervous system, leading to diverse neurological malfunction. (10)
 “My doctor says gluten is not a problem unless I have celiac disease”
“My doctor says gluten is not a problem unless I have celiac disease”
This is simply not true. Look at all the health problems gluten sensitivity can cause unrelated to celiac disease! In fact, as you can see, this can often be worse! Once a person develops gluten sensitivity without enteropathy (gastrointestinal disease), there is high risk of damage to the brain and nervous system.
A recent paper entitled “Gluten sensitivity: from gut to brain,” concluded that non-celiac gluten sensitivity is more likely to attack the brain and nervous system than any other organ:
“Thus, scientific literature now shows that gluten-immune reactions or gluten sensitivity not associated with the strict diagnostic criteria of celiac disease is more likely to attack the brain and nervous system than any other tissue”(11)
Gluten sensitivity is recently being found to be involved in the pathological processes of neurodegenerative diseases such as Alzheimer’s disease, Parkinson’s disease, supranuclear palsy, and Huntington’s disease:
“In this review, we discuss the molecular mechanisms of the transglutaminases involved in the pathological processes responsible for neurodegenerative diseases such as Alzheimer’s disease, Parkinson’s disease, supranuclear palsy, Huntington’s disease, and other recently identified polyglutamine diseases”(12)
Unfortunately, many medical doctors and other healthcare providers are not aware of this. How can this not be considered a problem?
 How common is gluten sensitivity?
How common is gluten sensitivity?
We are currently seeing a huge explosion in gluten sensitivity in this country leading to a wide variety of symptoms affecting multiple organ systems as seen above. These symptoms can range from mild to severe. But how common is it? We don’t really know at this point how common gluten sensitivity actually is. However, we do know that problems with gluten are widely underdiagnosed.
“…for every symptomatic patient with celiac disease there are eight patients with celiac disease and no gastrointestestinal symptoms” (13)
We also know that approximately 1/3 of the U.S. population has the HLA-DQ2 or DQ8 genotype (the genotype associated with celiac disease). This means that incidence of gluten sensitivity may be as high as 1/3 of the American population! It has been estimated that between 35-50% of the U.S. population has some form of gluten sensitivity. (14) Unfortunately, most of these patients go years suffering from various symptoms without a clear diagnosis.
“Many patients with undiagnosed celiac disease spend years seeking help for complaints such as chronic tiredness or mild abdominal symptoms”
“The response to an appropriate gluten-free diet is often life-transforming for symptomatic patients”(15)
 Where does gluten come from?
Where does gluten come from?
Gluten comes from wheat, barley and rye and is used extensively by the food industry because it is an extremely cheap food and can be used easily to produce a wide variety of food products. Almost anything that comes from a box or a bag contains gluten, including chips, crackers, cookies, cake, pasta, bread, cereal, frozen food, etc.
Common Sources of Gluten:
- Wheat
- Spelt
- Kamut
- Oats (98% of the oats in the U.S. are contaminated with gluten)
- Rye
- Barley
 There are also many hidden sources of gluten:
There are also many hidden sources of gluten:
- Soy sauce
- Food starches
- Food emulsifiers
- Food stabilizers
- Artificial food coloring
- Malt extract, flavor, syrup
- Dextrins
Why are we seeing such an increase in gluten sensitivity?
No one knows for sure why we are seeing this explosion of gluten sensitivity in the U.S.
But based on the fact that many gluten intolerant individuals can consume gluten in other countries, there is strong suspicion that the increased sensitivity to gluten in the U.S. is related to the production, processing and storage of gluten that are unique to this country. (16) The following is a list of likely culprits to the dramatic increase in gluten sensitivity we are now seeing across the country:
 Probable factors leading to increased prevalence of gluten sensitivity:
Probable factors leading to increased prevalence of gluten sensitivity:
- Hybridization of gluten
- Gluten deamidation
- Storage of grains
- Leaky gut syndrome
 Hybridization of Gluten
Hybridization of Gluten
The grains we consume now are not the same grains we used to consume as children or that our parents consumed: they are now hybridized foods. These are completely different grains and proteins. Hybridization involves cross-breeding various species. Gluten is not technically genetically modified, but it has been significantly hybridized and deamidated. (17, 18, 19) Hybridization is the process of creating a new protein by combining different strains of wheat together, not the process of inserting or deleting genes associated with genetic modification. This may create as much as 5% of new protein sequences in the new strain that are not found in the original sources. Many people feel that the hybridization of wheat has created a “new wheat” and one that appears to be very immunoreactive, especially to the brain and nervous system.
 Gluten Deamidation
Gluten Deamidation
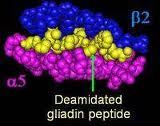
The other thing that has happened to our grains here in the U.S. is that the gluten we are now exposed to has undergone a process called deamidation. Deamidation of gluten is the product of chemical or enzymatic treatment of gluten used by the food-processing industry. This process is performed to make the food water soluble and easier to create food products from. However, people may have reactions to deamidated gliadin (the protein portion of gluten) but may not have reactions to gluten in its native form. (20) In one double-blinded, placebo-controlled study, subjects did not react to native wheat flour but had severe immune reactions to deamidated wheat. They concluded that gluten deamidation generates new immune-activating substances. (21)
Another study published in the European Journal of Inflammation concluded that deamidated glutens are “new” food compounds and may be the major cause of hidden inflammatory responses to food:
 “This extensive use of wheat isolates in the food industry may be the major cause of hidden food allergies…”
“This extensive use of wheat isolates in the food industry may be the major cause of hidden food allergies…”
“The wheat isolates are used as food emulsifiers, gelling agents, film formation aid, stretchability agents in meat products, sauces, soups and as clarifying agents in red wines”
“Because of food isolates or deamidated gluten are new food ingredients, when allergy to wheat is suspected, immune reaction to wheat isolates should be tested…”(22)
Overall, it is clear that although wheat does not fit the strict definition of a genetically-modified food (GMO), we are not longer consuming the wheat protein we used to eat and that the hybridization and deamidation of wheat protein are causing significant immune activation.
 Storage of Grains
Storage of Grains
The other thing that may account for this increase in gluten sensitivity is long-term storage of these grains in warehouses. The average grain is stored in bins for about 2 years before they are purchased by the food manufacturers. When it is stored in bins, enterotoxins (compounds toxic to the GI tract) tend to grow. These enterotoxins denature the proteins and are very inflammatory compounds. So the grains that are being consumed here in the U.S. are genetically-modified, deamidated, enterotoxin-filled grains. The outcome of this is that we now have a very inflammatory compound that is being used extensively throughout the food industry and is causing major problems in this susceptible population. (23)
Leaky Gut Syndrome
We will learn about the role that intestinal permeability or leaky gut syndrome plays in gluten sensitivity as well as the development of autoimmune disease in the next article in this series. It appears there is a vicious cycle that occurs between both gluten sensitivity and leaky gut syndrome increasing risk of autoimmune disease.
 How can I find out if I am gluten sensitive? Is lab testing for gluten sensitivity reliable?
How can I find out if I am gluten sensitive? Is lab testing for gluten sensitivity reliable?
Many patients are wondering if they are gluten sensitive and asking their doctors to test for this. Unfortunately, the conventional labs that are used by the majority of medical doctors testing for gluten sensitivity are not reliable. There are many false negative results, meaning, the results come back negative but the person is actually reacting to gluten. They are then being told by their doctors they can go ahead and eat wheat while they continue to suffer. Why is this?
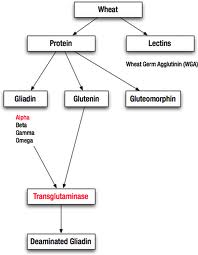 This is because all of these labs are using the same limited testing methods. They are only checking antibodies to one fraction of the wheat grain (gliadin) and only one type of gliadin (alpha gliadin) which is associated with celiac disease. However, there are many components that make up wheat that are causing immunological reactions, including, the protein portion (gluten) which is composed of gliadin and glutenin, and the lectin portion, including wheat germ agglutinin. In addition, the gliadin portion can be divided into alpha, gamma and omega gliadin. You can have an immune response to any of these fractions of wheat. But all conventional labs are currently only testing for alpha gliadin, not any of the other components to the wheat grain. Some labs are starting to check deamidated gliadin but again, only the alpha gliadin fraction. These labs are not testing for the whole spectrum of these immune responses to gluten or the lectin portion of wheat so most of these immunological reactions are being completely missed by the current conventional testing methods!
This is because all of these labs are using the same limited testing methods. They are only checking antibodies to one fraction of the wheat grain (gliadin) and only one type of gliadin (alpha gliadin) which is associated with celiac disease. However, there are many components that make up wheat that are causing immunological reactions, including, the protein portion (gluten) which is composed of gliadin and glutenin, and the lectin portion, including wheat germ agglutinin. In addition, the gliadin portion can be divided into alpha, gamma and omega gliadin. You can have an immune response to any of these fractions of wheat. But all conventional labs are currently only testing for alpha gliadin, not any of the other components to the wheat grain. Some labs are starting to check deamidated gliadin but again, only the alpha gliadin fraction. These labs are not testing for the whole spectrum of these immune responses to gluten or the lectin portion of wheat so most of these immunological reactions are being completely missed by the current conventional testing methods!
 Gluteomorphins
Gluteomorphins
Another response to wheat that is common, especially in the ADD/ADHD or autistic population of children, is a gluteomorphin response. Gluteomorphin is an opioid peptide that is formed during digestion of the gluten protein. Gluteomorphin responses are very common in those that have neurological or neurochemical responses to gluten exposure. This is a common problem in the autistic community. Gluten (from wheat) and casein (from dairy) get metabolized into opioids called gluteomorphin or caseomorphin and there is an immune reaction against it with this population of children. Many of these autistic kids are actually addicted to dairy and wheat. These compounds then cause neurochemical imbalances.
 Gluteomorphin Withdrawal Theory
Gluteomorphin Withdrawal Theory
One of the things that can happen with someone that has gluteomorphin antibodies, is they may have neurochemical imbalances induced and severe addiction to gluten. If they are put on a strict gluten-free diet, they are prone to develop a gluteomorphin withdrawal reaction. These individuals may feel worse and develop new symptoms when they start a gluten-free diet and symptoms may last a few days or several weeks. The reason for this is the gluteomorphin compound acts like an opioid in the brain. When this system gets disrupted, the opioid activity changes in their brain and in their enteric nervous system causing symptoms such as irregular bowel movements or severe depression or crazy thoughts.
 Prodynorphins
Prodynorphins
In addition to a gluteomorphin responses, people can also have a prodynorphin response. Prodynorphin is an opioid that is a basic building block of endorphins. Many people that have gluten immune reactions produce prodynorphin antibodies. Prodynorphin has been shown to play a part in many processes in the brain. These include how well people feel about themselves, their memories, and their perceptions of pain. It is known that people who don’t make enough prodynorphin (or have antibodies against them) are vulnerable to drug addiction, schizophrenia, bipolar disorders, and a form of epilepsy. (24, 25, 26, 27) Gluten sensitivity is known to lead to prodynorphin antibodies and potentially lead to neurochemical disorders. A person may have prodynorphin antibodies or gluteomorphin antibodies but they don’t have alpha gliadin antibodies. This means they will test negative on conventional lab testing for gluten sensitivity but eating gluten will totally throw off their brain chemistry!
 Is there any lab that offers reliable testing for gluten sensitivity?
Is there any lab that offers reliable testing for gluten sensitivity?
Yes, fortunately there is. Cyrex Labs (cyrexlabs.com) specializes in immunological testing and offers comprehensive gluten sensitivity testing which tests for immune reactions to all these components of wheat. Currently, only a small percentage of doctors and healthcare practitioners are using these specialized immunological testing methods so be sure to discuss this with your healthcare practitioner. Below is a description of the comprehensive wheat/gluten sensitivity testing that is available through Cyrex Labs.
Cyrex Array 3: Wheat/Gluten Proteome Sensitivity & Autoimmunity
Antibody Panel 3, called: “Wheat/Gluten Proteome Sensitivity & Autoimmunity” tests for IgA and IgG antibodies to all of the following wheat fractions. Antibodies to each of these fractions of wheat are involved in different immune reactions and have been associated with various symptoms and disease processes. For example, while transglutaminase 2 is involved in various gut reactions, transglutaminase 3 tends to be involved in various skin reactions and transglutaminase 6 is involved in various neurological problems. (28)
- Wheat

- Wheat germ agglutinin
- Deamidated gliadin 15
- Deamidated gliadin 17
- Deamidated gliadin 33
- Omega gliadin
- Glutenin
- Prodynorphin
- Gluteomorphin
- Transglutaminase 2
- Transglutaminase 3
- Transglutaminase 6
- Gliadin bound to transglutaminase
- Immune complexes
 Conclusion
Conclusion
Non-celiac gluten sensitivity is extremely common and widely underdiagnosed. Gluten sensitivity manifests in a wide range of symptoms that affect multiple organ systems of the body, not only the gastrointestinal tract. Celiac disease, which is one type of severe intolerance to gluten, was once believed to be primarily a gastrointestinal disorder, but this belief is now being challenged in the literature. Non-celiac gluten sensitivity is more likely to affect the brain and nervous system than the gastrointestinal system. Probable factors leading to the increased prevalence of gluten sensitivity include hybridization of wheat, deamidation of gluten and long-term storage of grains. Current conventional testing, although reliable for celiac disease, is not reliable for gluten sensitivity. There are reliable testing methods for gluten sensitivity available through Cyrex Labs. Be sure to discuss these testing methods with your doctor or healthcare practitioner if you suspect gluten sensitivity.
In part 5, we will discuss intestinal permeability (leaky gut syndrome)and how this condition is related to gluten sensitivity and the development of autoimmune disease.
References:
1. Kharrazian, D. The Gluten, Leaky Gut, Autoimmune Connection. Apex Energetics lecture. Mar. 16, 2013.
2. Murray, J. The widening spectrum of celiac disease. Am J Clin Nutr. 1999:69:354-65.
3. Increased prevalence and mortality in undiagnosed celiac disease. Gastroenterology. 2009 Jul;137(1):88-93. Epub 2009 Apr 10
4. Petersen V, Petersen R. The Gluten Effect: How “Innocent Wheat is Ruining Your Health”. True Health Publishing. 2009.
5. Hadjivassiliou M, et al. Gluten sensitivity as a neurological illness. J Neurol Neurosurg Psychiatry, 2007:72:560-563
6. Hadjivassiliou M, et al. Headache and CNS white matter abnormalities associated with gluten sensitivity. Neurology. 2001 Feb 13;56(3):385-388
7. Hernandez-Lahoz C, Mauri-Capdevila G, Vega-Villar J, Rodrigo L. [Neurological disorders associated with gluten sensitivity]. Rev Neurol. 2011 Sep 1;53(5):287-300.
8. Association between migraine and Celiac disease: results from a preliminary case-control and therapeutic study. Am J Gastroenterol. 2003 Mar;98(3)625-9.
9. A preliminary investigation of ADHD symptoms in persons with CD. J Atten Disord. 2006 Nov;10(2):200-4
10. Ford RP. The gluten syndrome: a neurological disease. Med Hypotheses. 2009 Sep;73(3):438-40
11. Hadjivassiliou M, et al. Gluten sensitivity: from gut to brain. Lancet Neurol. 2010 Mar;9(3):318-330
12. Transglutaminase-catalyzed post translational modifications of proteins in the nervous system and their possible involvement in neurodegenerative diseases. CNS Neurol Disord Drug Targets. 2008 Oct; 7(4):370-5.
13. Fasano A, Catassi C. Gastroenterology, 2001;120:636-651
14. Fine, Kenneth, “Early Diagnosis of Gluten Sensitivity: Before the Villi are Gone,” Celiac.com, http://www.celiac.com/articles/759/1/Early-Diagnosis-of-Gluten-Sensitivity-Before-the-Villi-are-Gone-By-Kenneth-Fine-MD/Page1.html.
15. Celiac disease: the great imitator. Med J Aust. 2004 May 17;180(10):524-526
16. Kharrazian, D. Understanding the Complexity of Gluten Sensitivity. Apex Energetics. Lecture. Jan. 27, 2011.
17. Yuan Z, et al. Mitototic illegitimate recombination is a mechanism for novel changes in high-molecular-weigh glutenin subunits in wheat-rye hybrids. PLoS One. 2011;6(8):e23511
18. Molnar-Lang M, et al. Identification and phenotypic description of new wheat : six-rowed winter barley disomic additions. Genome. 2012 Apr;55(4):302-311
19. Szakacs E, et al. Identification of new winter wheat—winter barley addition lines (6HS and 7H) using fluorescence in situ hybridization and the stability of the whole ‘Martonvasari 9 krl’- ‘Igri’ addition set. Genome. 2010 Jan;53(1):35-44.
20. Denery-Papini S, et al. Allergy to deamidated gluten in patients tolerant to wheat: specific epitopes linked to deamidation. Allergy. 2012 Aug;67(8):1023-32. doi: 10.1111/j.1398-9995.2012.02860.x. Epub 2012 Jun 28.
21. Anaphylaxis to wheat isolates: immunochemical study of a case proved by means of double-blind, placebo-controlled food challenge. J Allergy Clin Immunol. 2003 Apr; 111(4):897-899
22. The immunology of immediate and delayed hypersensitivity reaction to gluten. European Journal of Inflammation. 2008 Jan;6(1):1721-1727.
23. Kharrazian, D. The Gluten, Leaky Gut, Autoimmune Connection. Apex Energetics lecture. Mar.16, 2013.
24. Schwarzer C. 30 years of dynorphins–new insights on their functions in neuropsychiatric diseases. Pharmacol Ther. 2009 Sep;123(3):353-70. doi: 10.1016/j.pharmthera.2009.05.006. Epub 2009 May 28.
25. Butelman ER, Yuferov V, Kreek MJ. κ-opioid receptor/dynorphin system: genetic and pharmacotherapeutic implications for addiction. Trends Neurosci. 2012 Oct;35(10):587-96. doi: 10.1016/j.tins.2012.05.005. Epub 2012 Jun 16.
26. Hurd YL. Subjects with major depression or bipolar disorder show reduction of prodynorphin mRNA expression in discrete nuclei of the amygdaloid complex. Mol Psychiatry. 2002;7(1):75-81.
27. Peckys D, Hurd YL. Prodynorphin and kappa opioid receptor mRNA expression in the cingulate and prefrontal cortices of subjects diagnosed with schizophrenia or affective disorders. Brain Res Bull. 2001 Jul 15;55(5):619-24.
28. Cyrex Labs website. www.cyrexlabs.com