 In the last segment, we reviewed how our bodies eliminate the toxic chemicals we are exposed to on a daily basis and introduced the concept of “toxicant-induced loss of tolerance”. We also discussed some of the mechanisms that lead to this condition, which is becoming more and more common, as well as common signs and symptoms of this condition. In this final segment of this series, we discuss the role chemical sensitivity plays in the development of autoimmunity and laboratory evaluation of immune-chemical tolerance. We also consider other factors besides chemical exposure that impact chemical sensitivity. Then we discuss nutritional management of loss of chemical tolerance from a functional medicine perspective.
In the last segment, we reviewed how our bodies eliminate the toxic chemicals we are exposed to on a daily basis and introduced the concept of “toxicant-induced loss of tolerance”. We also discussed some of the mechanisms that lead to this condition, which is becoming more and more common, as well as common signs and symptoms of this condition. In this final segment of this series, we discuss the role chemical sensitivity plays in the development of autoimmunity and laboratory evaluation of immune-chemical tolerance. We also consider other factors besides chemical exposure that impact chemical sensitivity. Then we discuss nutritional management of loss of chemical tolerance from a functional medicine perspective.
Key concepts for this issue:
- The Role Chemical Sensitivity Plays in the Development of Autoimmunity
- Why Does Chemical Tolerance Vary From Person to Person?
- Laboratory Evaluation of Immune-Chemical Tolerance
- Other Factors Besides Chemical Exposure That Impact Chemical Sensitivity
- Nutritional Management of Loss of Chemical Tolerance
 The Role Chemical Sensitivity Plays in the Development of Autoimmunity
The Role Chemical Sensitivity Plays in the Development of Autoimmunity
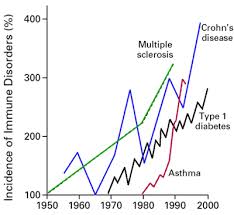
As discussed in previous segments, the prevalence of autoimmunity is increasing at an alarming rate.
“Currently 1 in 12 women and 1 in 25 men have autoimmune disease. Over 50 million Americans now have autoimmune disease”[47]
Additionally, the research points to chemicals as contributing factors to autoimmunity, cancer and neurological conditions:
 “There are increasing rates of autoimmunity, cancer, neurological disorders, and inflammatory conditions evoked by chemicals”[48]
“There are increasing rates of autoimmunity, cancer, neurological disorders, and inflammatory conditions evoked by chemicals”[48]
“Autoimmune diseases may be induced by physical and/or chemical environmental factors”[49]
Somewhere along the way after the depletion of glutathione, we turn on autoimmunity causing destruction of various tissues, including the brain, gut, thyroid and a number of other tissues. When we lose this glutathione system, we lose our capacity to handle environmental compounds and self-tolerance to our own tissue. But how does this happen?
 Prevailing theory of how chemical sensitivity leads to autoimmunity:
Prevailing theory of how chemical sensitivity leads to autoimmunity:
When environmental compounds enter the body, they often bind to proteins of human tissue such as albumin because this is how the body eliminates these compounds. A hapten is a small molecule that can elicit an immune response only when attached to a large carrier such as a protein. In some individuals, the immune system responds to this protein-bound hapten. When the immune system responds to this foreign antigen complex, it usually produces antibodies to the human tissue portion, rather than the hapten so the immune response continues even after the hapten is removed. Depending on the human tissue that becomes targeted by the immune system, various autoimmune conditions can result.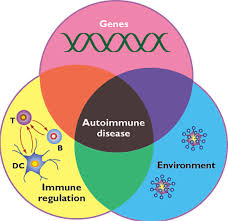
“Epidemic clustering of some autoimmune diseases following xenobiotic exposure reinforces the thesis that autoimmune disease is secondary to genetic and environmental factors”[50]
“Basic science and epidemiological research suggests that oxidative stress and inflammation may play a role in autoimmune disease”[51]
Why Does Chemical Tolerance Vary From Person to Person?
 Why are most people living relatively normal, healthy lives despite all these toxic exposures while other people succumb to toxin-induced illness? If you tested random people in the U.S., including healthy people, chances are all of them would show contamination from heavy metals and environmental chemicals. Being completely free of heavy metals and environmental chemicals these days is impossible. Anthropological studies show even mummies were contaminated with heavy metals. Our bodies have the capacity to deal with chemical and heavy metal exposure by either eliminating these from the body following transformation via the liver and excretion via the urine or stool, or in some cases, sequestering heavy metals in tissue, such as bone.
Why are most people living relatively normal, healthy lives despite all these toxic exposures while other people succumb to toxin-induced illness? If you tested random people in the U.S., including healthy people, chances are all of them would show contamination from heavy metals and environmental chemicals. Being completely free of heavy metals and environmental chemicals these days is impossible. Anthropological studies show even mummies were contaminated with heavy metals. Our bodies have the capacity to deal with chemical and heavy metal exposure by either eliminating these from the body following transformation via the liver and excretion via the urine or stool, or in some cases, sequestering heavy metals in tissue, such as bone.
 Some people seem to have immune responses to these environmental compounds, while others do not. In fact, one person can have very high levels of toxicity and be symptom-free, while another person who has low levels of contamination reacts severely. The issue is not how many toxins are in your system but whether your immune system reacts to them. This can cause severe reactions and symptoms and lead to chronic inflammation. This is the mechanism behind toxicant-induced loss of chemical tolerance (TILT), multiple chemical sensitivities, and toxin-induced brain degeneration mechanisms that are becoming so common today. How do we evaluate loss of chemical tolerance?
Some people seem to have immune responses to these environmental compounds, while others do not. In fact, one person can have very high levels of toxicity and be symptom-free, while another person who has low levels of contamination reacts severely. The issue is not how many toxins are in your system but whether your immune system reacts to them. This can cause severe reactions and symptoms and lead to chronic inflammation. This is the mechanism behind toxicant-induced loss of chemical tolerance (TILT), multiple chemical sensitivities, and toxin-induced brain degeneration mechanisms that are becoming so common today. How do we evaluate loss of chemical tolerance?
Laboratory Evaluation of Environmental Chemical Tolerance
Evaluating chemical immune tolerance can be done objectively with Cyrex Labs Array 11—Chemical Immune Reactivity Screen. Chemical immunoreactivity testing evaluates for immunological reactivity to environmental compounds by evaluating antigen-antibody reactivity to these compounds. The presence of elevated antibodies to common environmental compounds indicates overzealous immune reactions to chemicals and loss of immune tolerance. Chemical antibody testing has several advantages. First, it allows for a diverse array of common chemicals to be evaluated, in addition to heavy metals. Second, it measures immune responses to these chemicals, unrelated to their quantitative load, that result in immunological and inflammatory responses from these environmental chemicals. Elevated chemical antibodies indicate an exaggerated immune response to these common chemicals leading to the promotion of systemic inflammation and can occur with trace exposures of chemicals when immune integrity is compromised. Any elevation in chemical antibodies indicate loss of chemical tolerance and risk of abnormal immune reactions to everyday environmental compounds.
Are There Factors Besides Chemical Exposure That Impact Chemical Sensitivity?
Unrelated to environmental loads, you can lose chemical tolerance from the following immunological imbalances:
- Chronic stress

- Intestinal permeability
- Chronic infections
- Chronic inflammation
- Autoimmunity
- Poor sleep
- Malnutrition
Chemical sensitivity can be impacted by all of these factors unrelated to toxin exposures. For example, patients exposed to chronic stress may lose the integrity of their barrier systems and develop insufficiency of their immune regulatory T-cells as a result. They may then start to react immunologically to daily chemical exposures such as cigarette smoke or gasoline fumes. The exposure may cause them to suffer migraines, skin outbreaks, sinus reactions, etc. In this case, addressing the person’s internal stress response with stress management and nutritional compounds (ie: adaptogens, etc.) is critical to minimizing the factors promoting the person’s stress physiology and chemical sensitivity.
 Another example of a condition that can affect chemical sensitivity is chronic infection. Chronic infection can lead to chronic inflammation and compromised immune regulatory T-cell function as well as loss of barrier system integrity. When your immune system is constantly working 24/7 to eliminate a pathogen but is unsuccessful, it is at risk of loss of regulatory T-cell function and dysfunctional immune responses. This is what happens in certain chronic infections such as chronic Lyme disease when the instigating pathogen (a bacteria called borellia burgdorferi and other concomitant co-infections) cannot be eliminated by the immune system. The individual eventually becomes at risk for chemical intolerance and autoimmune reactions. Autoimmune conditions always involve a certain degree of chronic inflammation and T-regulatory cell dysfunction as well which can then lead to loss of chemical tolerance. These types of issues must be identified and addressed in order to have a chance at improving tolerance to environmental chemicals. Otherwise, progress will be very limited and palliative at best. It is important the practitioner consider all of the potential contributors that may play a role in loss of chemical tolerance.
Another example of a condition that can affect chemical sensitivity is chronic infection. Chronic infection can lead to chronic inflammation and compromised immune regulatory T-cell function as well as loss of barrier system integrity. When your immune system is constantly working 24/7 to eliminate a pathogen but is unsuccessful, it is at risk of loss of regulatory T-cell function and dysfunctional immune responses. This is what happens in certain chronic infections such as chronic Lyme disease when the instigating pathogen (a bacteria called borellia burgdorferi and other concomitant co-infections) cannot be eliminated by the immune system. The individual eventually becomes at risk for chemical intolerance and autoimmune reactions. Autoimmune conditions always involve a certain degree of chronic inflammation and T-regulatory cell dysfunction as well which can then lead to loss of chemical tolerance. These types of issues must be identified and addressed in order to have a chance at improving tolerance to environmental chemicals. Otherwise, progress will be very limited and palliative at best. It is important the practitioner consider all of the potential contributors that may play a role in loss of chemical tolerance.
 Management of Loss of Chemical Tolerance
Management of Loss of Chemical Tolerance
Management of loss of chemical tolerance involves:
- Identification of offending chemicals/heavy metals (through laboratory evaluation)
- Avoidance or minimization of exposures to these offending chemicals/heavy metals from one’s environment (as much as possible)
- Nutritional support of the physiologic systems involved in loss of chemical tolerance
- Targeted nutritional support for phase I and phase II biotransformation pathways for transformation and elimination of offending chemicals (when applicable)
 Avoiding Exposures
Avoiding Exposures
Knowing common environmental sources of exposure of these chemical compounds that initiate immune responses is a critical first step in order to minimize these exposures and resultant “flareups” of symptoms. Avoiding these compounds completely cannot always be done in all cases but many of these compounds can often be avoided and avoidance alone can sometimes lead to significant improvement in symptoms. For example, common sources of mercury exposures include amalgam fillings and medical implants, vaccinations and contaminated fish and shellfish and contaminated fish oils. Consideration should be given to removal of dental amalgums (by a qualified dentist in an appropriate way) and vaccination schedules. Decreased frequency or decreased regularity of vaccinations can minimize impact of exposures. Fish consumption can be a source of exposure as well, as discussed earlier. Limiting fish consumption to twice a week and consuming only wild fish rather than farm-raised fish can significantly decrease risk of mercury exposures. Quality fish oils produced by a reputable company that tests for mercury levels (which tend to cost a little more than some of the cheaper supplements) are recommended. Look for levels of detectability of heavy metals, such as mercury, lead, PCBs and dioxins in ppb (parts per billion) and ppt (parts per trillion).
 Nutritional Support for Chemical Tolerance
Nutritional Support for Chemical Tolerance
Immune-chemical tolerance is dependent upon many overlapping physiological factors that include the glutathione system, regulatory T-cell function, barrier system integrity, NF-kB dysregulation and chronic inflammation and impaired hepatic biotransformation.
- Depletion of glutathione and inadequate glutathione system
- Regulatory T-cell failure
- Breakdown of barrier systems
- NF-kB dysregulation/chronic inflammation
- Impaired hepatic biotransformation
All of these systems are compromised to some degree in loss of chemical tolerance and management of this condition must include assessment of all these areas and address all physiological imbalances that are identified or suspected. There are various natural compounds that have been shown in the scientific literature to address each of these physiologic imbalances which can have powerful effects. These are the compounds we use in functional medicine to improve chemical tolerance. Here are the primary strategies we use and a brief list of the main compounds used to support each of these systems.
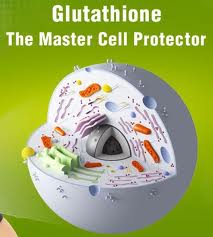
 Optimize Glutathione and Glutathione System
Optimize Glutathione and Glutathione System
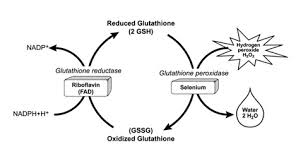
Glutathione helps support regulatory T cells, and differentiation of T-cells into their specific types by reducing damage from oxidative stress. This system is absolutely critical for overall modulation of immune responses. There are several compounds that have been identified in the literature to help raise intracellular glutathione, activate the glutathione peroxidase and reductase enzymes, and support the glutathione system.
 N-acetyl-cysteine
N-acetyl-cysteine
N-acetyl-cysteine is a metabolite of the sulfur-containing amino acid, cysteine. It plays a role in the sulfation cycle, acting as a sulfur donor in phase II detoxification and as a methyl donor in the conversion of homocysteine to methionine. N-acetyl cysteine is rapidly metabolized to intracellular glutathione. It is used for acetaminophen overdose and as a nephroprotective agent for radiocontrast. [52-58]
 Alpha lipoic acid
Alpha lipoic acid
Alpha lipoic acid is an antioxidant that is made by the body and is found in every cell, where it helps turn glucose into energy. Unlike other antioxidants, which work only in water (such as vitamin C) or fatty tissues (such as vitamin E), alpha lipoic acid is both fat- and water-soluble. This means it can work throughout the body. Alpha lipoic acid also plays an important role in the synergism of antioxidants. It directly recycles and extends the metabolic life spans of vitamin C, glutathione, and coenzyme Q10, and it indirectly renews vitamin E, all of which are necessary for glutathione recycling. [59-68]
 L-glutamine
L-glutamine
L-glutamine is important for the generation of glutathione stores since glutamate is unable to be transported into cells. Glutamine is efficiently transported into the cell, converted to glutamate, and readily available for glutathione synthesis. Research has demonstrated that glutamine is important for the generation of glutathione. [69-82]
 Selenium
Selenium
Selenium is a trace element nutrient that serves as the essential cofactor for the enzyme glutathione peroxidase. Selenium-deficient humans and animals are known to be deficient in glutathione peroxidase activity in their cells and plasma. [83-94]
 Cordyceps
Cordyceps
Cordyceps (used in Chinese medicine for thousands of years) has been shown to activate glutathione peroxidase synthesis in the body (the enzymes that increase glutathione) and raise glutathione levels within minutes. Research has demonstrated cordyceps helps protect cells by engaging the glutathione enzyme cycle. [95-98]
 Centella asiatica (Gotu Kola)
Centella asiatica (Gotu Kola)
Research has clearly demonstrated that oral intake of gotu kola very rapidly and dramatically increases the activity and amount of glutathione peroxidase and quantity of glutathione. [99-109]
 Silybum marianum
Silybum marianum
Administration of Silybum marianum has shown to significantly increase glutathione, increase superoxide dismutase activity, and have positive influence in the ratios of reduced and oxidized glutathione. [110-126]
 Broccoli extract
Broccoli extract
Broccoli has a high content of glucosinolates, which are metabolized into isothiocyanates and sulforaphane [127]. These compounds exhibit chemoprotective activity through a mechanism involving inhibition of cytochrome P450 and induction of GST and other enzymes. [128,129]
 Optimize Regulatory T-Cell Function and TH-3 System
Optimize Regulatory T-Cell Function and TH-3 System
The two most powerful ways known to support regulatory T-cell function and coordinate TH-1 and TH-2 balance involve glutathione and vitamin D.
 Glutathione
Glutathione
Glutathione (GSH) is one of the most critical immune-modulating substances that we know of. Like a conductor of an orchestra, glutathione regulates various aspects of immune balance. As previously discussed, studies show that GSH has a significant impact on the immune system’s ability to activate the appropriate T-helper cell response. [130,131] Because GSH is so important in the immune system’s activation of the appropriate T-helper response, altering its levels may have significant implications in TH1/TH2-related diseases. [132]
“Accumulation of evidence suggests that intracellular GSH (glutathione) levels in antigen-presenting cells such as macrophages, influence the TH1/TH2 cytokine response pattern. The observations reported herein show that pro-GSH molecules represent new therapeutic agents to support immune modulation.” [133]
“These data indicate that glutathione peroxidase-dependent control of intracellular reactive oxygen species accumulation is important not only for regulation of TH-cell proliferation, but also for modulation of differentiation into TH1, TH2 and TH17 cells.”[134]
See the clinical strategies described above for strategies for increasing glutathione levels.
 Vitamin D
Vitamin D
Numerous studies have been published establishing the critical immunoregulatory role that vitamin D plays in the prevention of immune dysfunction and the development of autoimmune disease. [135-142] Vitamin D appears to act on a number of different immune cells to promote various regulatory responses by the immune system. Vitamin D deficiency has been associated with many autoimmune disorders including multiple sclerosis, Type 1 diabetes, Crohn’s disease, rheumatoid arthritis as well as others. [143]
Studies have shown a significant relation between vitamin D deficiency and allergy and an important role of vitamin D in the pathogenesis and severity of allergic disease, and its capacity to control allergic disease. [144,145] Vitamin D supplementation has been shown to reduce the occurrence of asthma in most related studies and may be useful in the prevention or adjunct treatment of chronic obstructive pulmonary disease. [146,147]
Here are a few selections from the literature on the role vitamin D plays in immune health:
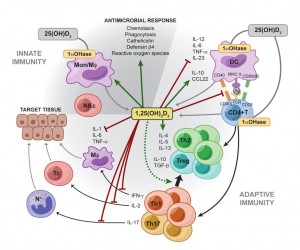 “Increasing evidence demonstrates a strong association between vitamin D signaling and many biological processes that regulate immune responses. The discovery of the vitamin D receptor in multiple immune cell lineages, such as monocytes, dendritic cells, and activated T cells credits vitamin D with a novel role in modulating immunological functions and its subsequent role in the development or prevention of autoimmune diseases.”[148]
“Increasing evidence demonstrates a strong association between vitamin D signaling and many biological processes that regulate immune responses. The discovery of the vitamin D receptor in multiple immune cell lineages, such as monocytes, dendritic cells, and activated T cells credits vitamin D with a novel role in modulating immunological functions and its subsequent role in the development or prevention of autoimmune diseases.”[148]
“It is apparent that vitamin D has significant effects on the immune system and as such may contribute to the pathogenesis of autoimmune disease. Low vitamin D status is reported in many inflammatory rheumatic conditions. In some this extends to an association with disease activity. Vitamin D acts on a number of cells involved in both innate and acquired immunity biasing the adaptive immune system away from Th17 and Th1, towards Th2 and T-regs (T3). Deficiency accordingly could encourage autoimmunity. Vitamin D deficiency may well be an important factor in autoimmune rheumatic disease, including initial disease development and worsening the disease once present.”[149]
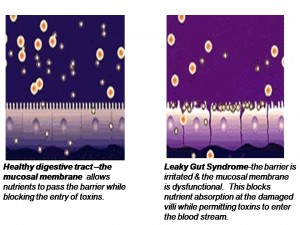 Optimize Protective Barrier Systems
Optimize Protective Barrier Systems
Most people with loss of chemical tolerance have a compromised intestinal barrier. Improving the integrity of this barrier is critical to minimizing inflammatory responses. There are a number of compounds which have been shown to improve the integrity of the body’s intestinal barrier system.
L-Glutamine
L-glutamine is the preferred fuel source for the cells of the small intestine and has been shown in numerous studies to support the regeneration and repair of the intestinal lining. It has also been shown to increase the number of cells in the small intestine, the number of villi on those cells, as well as the height of the villi. Glutamine-reduced permeability of the lining may accompany “leaky gut” patterns that promote intestinal inflammation and the development of delayed food intolerances. [150-171]
 Deglycyrrhizinated Licorice
Deglycyrrhizinated Licorice
Deglycyrrhizinated licorice is a popular and substantially studied natural compound that provides flavonoids that help heal the gastric and intestinal lining. Many different mechanisms have been shown with regard to its restorative properties including stimulation and differentiation of glandulars cells, protective mucous formation, protective mucous secretion, increased intestinal blood flow, and growth and regeneration of intestinal lining cells. [172-189]
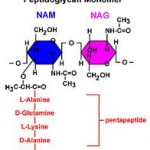 N-Acetyl Glucosamine
N-Acetyl Glucosamine
N-acetyl glucosamine is a monosaccharide derivative of glucose that is used to support the intestinal glycoprotein cover of the mucosa called mucin. It is also a precursor substrate for the repair of the intestinal mucosal cells and provides support of mucosa membrane irritation. [190-193]
 Aloe Leaf Extract
Aloe Leaf Extract
Aloe leaf extract contains natural phytochemicals and powerful antioxidant properties that reduce intestinal inflammation, soothe the intestines, aid in intestinal wound healing, and have an anti-ulcer effect. It also appears to have antifungal properties, supports cholinergic intestinal motility, and reduces intestinal pain and discomfort. [194-203]
 Spanish Moss
Spanish Moss
Spanish moss is also known as Tillandsia and it has historically been used for intestinal irritation and allergies. Research on the plant has identified rich sources of flavonoids and other phytochemicals that provide antimicrobial activity and free radical scavenging properties. [204-209]
 Marshmallow Extract
Marshmallow Extract
Marshmallow extract has high content of mucilage that can soothe and help heal compromised intestinal barrier tissue. It is also rich in antioxidants that can support healing of tissue. It also has properties that inhibit hyaluronidase, which is the enzyme involved in the production of hyaluronic acid that is involved with intestinal tissue destruction. [210-213]
 Methylsulfonylmethane (MSM)
Methylsulfonylmethane (MSM)
Methylsulfonylmethane (MSM) is a rich source of natural sulfur which helps as a substrate for antioxidant defense systems as well as support substrates for hepatic phase II sulfation pathways. It has antifungal and anti-inflammatory properties that help support the compromised liver-gut axis. [214-218]
 Gamma Oryzanol
Gamma Oryzanol
Gamma oryzanol is a mixture of plant sterols and ferulic acid esters from rice. It has demonstrated to be a powerful antioxidant. Numerous papers have demonstrated its effectiveness in gastrointestinal complaints, ulcers, irritable bowel syndrome and non-specific gastrointestinal conditions. It has also been shown to modulate and support the enteric nervous system in its ability to activate intestinal motility and secrete digestive enzymes. [219-226]
 Slippery Elm Bark
Slippery Elm Bark
Slippery elm bark is very high in natural mucilage and helpful in soothing the inflamed intestinal cells. It reduces contact of inflammatory proteins with the intestinal mucosa, thereby enhancing recovery from intestinal barrier compromise and inflammation. [227-230]
 German Chamomile
German Chamomile
The chief constituents of German chamomile have been shown to enhance wound-healing time, modulate prostaglandins and nitric oxide activity to provide gastric and intestinal protection. [231-238]
 Marigold Flower Extract
Marigold Flower Extract
Marigold flower extract constituents include saponins, carotenoids, flavonoids, mucilage, bitter principle, phytosterols, polysaccharides, and resin. It has been used historically for varied gastrointestinal complaints. It provides substrates for digestive enzyme production, helps during inflammation and provides antibacterial activity. [239-246]
 Glutathione
Glutathione
When a person loses their ability to recycle glutathione and glutathione levels become depleted, they are at risk for intestinal lining inflammation which then leads to leaky gut. The glutathione recycling system is one of the main systems that prevents leaky gut onset. Glutathione is suggested to play an important role in gut barrier function and prevention of intestinal inflammation. [247-252]
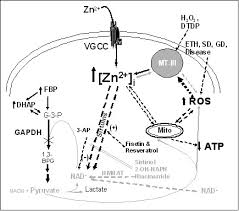
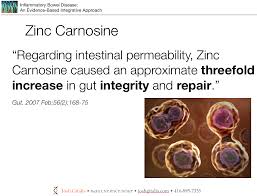 Zinc Carnosine
Zinc Carnosine
“Regarding intestinal permeability, zinc carnosine caused an approximate threefold increase in gut integrity and repair”[253]
Vitamin D
“VDR (vitamin D receptor) plays a critical role in mucosal barrier homeostasis by preserving the integrity of junction complexes and the healing capacity of the colonic epithelium. Therefore, vitamin D deficiency may compromise the mucosal barrier, leading to increased susceptibility to mucosal damage and increased risk of IBD (inflammatory bowel disease).”[254]
 “There is growing appreciation of the importance of the pleiotropic hormone vitamin D in the development of tolerance, immune system defenses, and epithelial barrier integrity” [255]
“There is growing appreciation of the importance of the pleiotropic hormone vitamin D in the development of tolerance, immune system defenses, and epithelial barrier integrity” [255]
“1,25(OH)2D3 (vitamin D) may play a protective role in mucosal barrier homeostasis by maintaining the integrity of junction complexes and in healing capacity of the colon epithelium. 1,25(OH)2D3 may represent an attractive and novel therapeutic agent for the adjuvant therapy of IBD (inflammatory bowel disease).”[256]
 Intestinal Permeability Dietary Restrictions
Intestinal Permeability Dietary Restrictions
It is important to avoid certain types of food that tend to aggravate or worsen intestinal permeability when trying to repair the gut barrier and decrease autoimmune responses. These self-promoting vicious cycles become difficult to unwind unless aggressive dietary and nutritional strategies are employed. See Intestinal Permeability Dietary Restrictions at the end of Successful Aging Part 6b for a complete list of these foods.
Optimize NF-kB Activity and Minimize Chronic Inflammation
NF-kB signaling needs to be downregulated in order to maintain tissue homeostasis. Overall, it appears that the two most potent natural NF-kB minimizers that researchers have discovered are curcumin and resveratrol. Curcumin is the alkaloid derived from turmeric, a spice used in Indian cooking. Resveratrol is a compound found in the skin of red grapes, peanuts and some berries. In recent studies, both curcumin and resveratrol have shown to support healthy numbers of T-cell cytokines (inflammatory messengers). These results suggest the potential use of these phytochemicals for supporting healthy immune responses. Here is what some recent literature is saying about these compounds:
 Curcumin
Curcumin
“Curcumin, a dietary spice from turmeric, has outstanding anti-inflammation and neuroprotective effects. Herein, we review key features of curcumin involved in biology, pharmacology, and medicinal chemistry and discuss its potential relevance to pathophysiological progress of multiple sclerosis”[257]
“Curcumin, a component of turmeric, has been shown to be non-toxic, to have antioxidant activity, and to inhibit such mediators of inflammation as NFkB, cyclooxygenase-2 (COX-2), lipooxygenase (LOX), and inducible nitric oxide synthase (iNOS)”[258]
“In a larger, randomized, double-blind, multicenter trial involving patients with quiescent ulcerative colitis, administration of 1 g of curcumin twice daily resulted in both clinical improvement and a statistically significant decrease in the rate of relapse”[259]
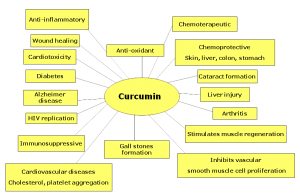 “Our results indicate that curcumin has the potential to protect against cardiac inflammation… and may provide a novel therapeutic strategy for autoimmune myocarditis” [260]
“Our results indicate that curcumin has the potential to protect against cardiac inflammation… and may provide a novel therapeutic strategy for autoimmune myocarditis” [260]
“In various chronic illnesses in which inflammation is known to play a major role, curcumin has been shown to exhibit therapeutic potential. These diseases include Alzheimer’s disease (AD), Parkinson’s disease, multiple sclerosis, epilepsy, cerebral injury, CVDs, cancer, allergy, asthma, bronchitis, colitis, rheumatoid arthritis, renal ischemia, psoriasis, diabetes, obesity, depression, fatigue, and AIDS”[261]
“…curcumin has received considerable interest as a potential therapeutic agent for the prevention and/or treatment of various malignant diseases, arthritis, allergies, Alzheimer’s disease, and other inflammatory illnesses. The underlying mechanisms of these effects are diverse and appear to involve the regulation of various molecular targets, including transcription factors (such as nuclear factor-kB)…”[262]
 Resveratrol
Resveratrol
Resveratrol has been shown in the literature to have powerful anti-inflammatory effects which involve multiple pathways including inhibiting NF-kB, inhibiting iNOS (inducible-nitric oxide synthase) expression and inhibiting inflammatory cytokines such as IL-6 in various inflammatory conditions, including multiple sclerosis [263], diabetic neuropathy [264], arthritis [265], autoimmune myocarditis [266], colitis [267], and exerts immunomodulatory effects both in vitro and in vivo in lymphocytic leukemia. [268]
“These studies demonstrate that SRT501 (a pharmaceutical grade formulation of resveratrol) attenuates neuronal damage and neurological dysfunction in experimental autoimmune encephalomyelitis (the animal model of multiple sclerosis) by a mechanism involving SIRT1 activation”[269]
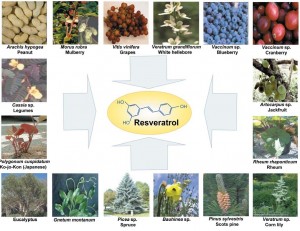 “This study confirms the NF-kB inhibitory activity and anti-inflammatory activity of resveratrol, which may contribute to neuroprotection in diabetic neuropathy apart from its antioxidant effect”[270]
“This study confirms the NF-kB inhibitory activity and anti-inflammatory activity of resveratrol, which may contribute to neuroprotection in diabetic neuropathy apart from its antioxidant effect”[270]
“In summary, our results suggest that resveratrol suppresses apoptosis and inflammatory signaling through its actions on the NF-kB pathway in human chondrocytes”[271]
“Resveratrol significantly ameliorated myocardial injury and preserved cardiac function in a rat model of autoimmune myocarditis” [272]
 In addition, both curcumin and resveratrol have been shown to reduce the inflammatory mediators that contribute to the low-level, chronic inflammation found in obese individuals and have been linked to the onset of cardiovascular disorders, insulin resistance and type 2 diabetes mellitus.
In addition, both curcumin and resveratrol have been shown to reduce the inflammatory mediators that contribute to the low-level, chronic inflammation found in obese individuals and have been linked to the onset of cardiovascular disorders, insulin resistance and type 2 diabetes mellitus.
“Curcumin and resveratrol are able to inhibit TNFalpha-activated NF-kappaB signaling in adipocytes and as a result significantly reduce cytokine expression. These data suggest that curcumin and resveratrol may provide a novel and safe approach to reduce or inhibit the chronic inflammatory properties of adipose tissue.”[273]
Optimize Targeted Phase I and Phase II Hepatic Biotransformation Pathways
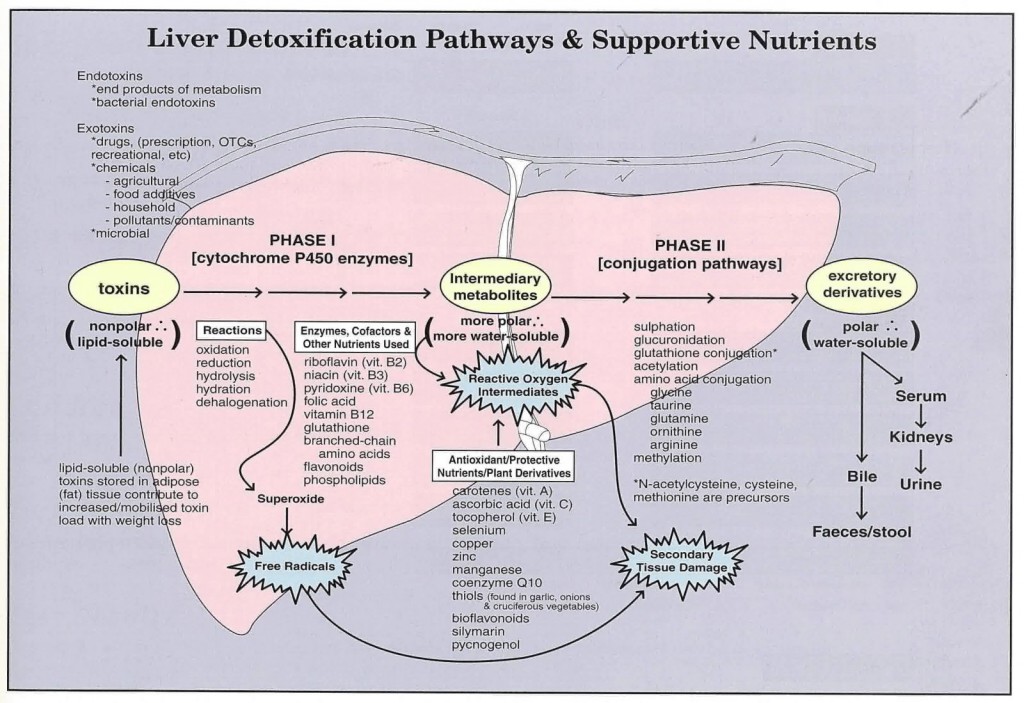 As discussed above, both phase I and phase II hepatic biotransformation pathways are involved in transformation and elimination of environmental chemicals. Phase I reactions involve the cytochrome P450 enzyme which is responsible for converting lipophilic (fat-loving) toxins into biotransformed intermediates that are more water-soluble. In phase II, these biotransformed intermediates undergo further biotransformation in a second series of enzymes called conjugases. Each chemical we are exposed to is eliminated from the body via specific phase II pathways. This means it is most efficient to support those specific detox pathways that are involved in the elimination of the particular chemicals that are responsible for the immune reactions and increase of symptoms as identified by laboratory testing. It is important to note that heavy metals do not enter phase I and phase II biotransformation pathways.
As discussed above, both phase I and phase II hepatic biotransformation pathways are involved in transformation and elimination of environmental chemicals. Phase I reactions involve the cytochrome P450 enzyme which is responsible for converting lipophilic (fat-loving) toxins into biotransformed intermediates that are more water-soluble. In phase II, these biotransformed intermediates undergo further biotransformation in a second series of enzymes called conjugases. Each chemical we are exposed to is eliminated from the body via specific phase II pathways. This means it is most efficient to support those specific detox pathways that are involved in the elimination of the particular chemicals that are responsible for the immune reactions and increase of symptoms as identified by laboratory testing. It is important to note that heavy metals do not enter phase I and phase II biotransformation pathways.
 Phase I pathways are primarily dependent on the glutathione system as well as the cytochrome P450 enzyme system, therefore, the glutathione system is always supported in all chemical exposures. Phase II pathways rely on different enzymes with various coenzymes and cofactors needed to function properly. There are a number of key compounds that have been identified to support each of these specific pathways, including sulfation, methylation, glutathione conjugation, acetylation, glucoronidation and glycine (amino acid) conjugation. In addition, there are a number of natural compounds that have been shown to support bile formation and secretion and excretion of toxic compounds through the biliary system, known as phase III pathways.
Phase I pathways are primarily dependent on the glutathione system as well as the cytochrome P450 enzyme system, therefore, the glutathione system is always supported in all chemical exposures. Phase II pathways rely on different enzymes with various coenzymes and cofactors needed to function properly. There are a number of key compounds that have been identified to support each of these specific pathways, including sulfation, methylation, glutathione conjugation, acetylation, glucoronidation and glycine (amino acid) conjugation. In addition, there are a number of natural compounds that have been shown to support bile formation and secretion and excretion of toxic compounds through the biliary system, known as phase III pathways.
 Dandelion (Taraxacum officinale)
Dandelion (Taraxacum officinale)
Dandelion root has physiologic impacts on both the liver and gallbladder. It impacts the liver by promoting the production of bile and its delivery to the gallbladder. It impacts the gallbladder by causing contraction and release of stored bile.[274-276]
 Milk Thistle (Silybum marianum)
Milk Thistle (Silybum marianum)
Milk thistle has the ability to increase the solubility of bile and its use has been shown to significantly reduce biliary cholesterol concentrations and bile saturation index.[277] It has potent antioxidant activity which supports phase I detoxification and prevents the depletion of hepatic glutathione which is important for phase II detoxification.[278-280] Silybum marianum has anti-inflammatory chemical properties that are inhibitors of inflammatory prostaglandins and leukotrienes as well as chemical properties that promote protein synthesis to replace damaged liver cells. [281-284]
 Gotu Kola (Centella asiatica)
Gotu Kola (Centella asiatica)
Gotu kola has active constituents known as triterpenoid compounds that have impacts on cells and tissues that are important in detoxification. It has shown the ability to improve histological findings of liver cirrhosis.[285,286] It also supports hepatic detoxification due to its physiological impact on enhancing venous circulation. Centella asiatica has shown the ability to improve venous disorders such as chronic venous insufficiency and venous hypertension.[287,288] Improved venous circulation has influential roles in optimizing detoxification that are generally overlooked.
 Panax Ginseng
Panax Ginseng
Panax ginseng has shown in several studies to have numerous positive impacts on hepatic function. It has shown to reverse fatty liver in animals, and demonstrate profound anti-hepatotoxic properties.[289,290] It has shown the ability to promote Kupffer cells and shown to increase nuclear, ribosomal, and messenger RNA biosynthesis. [291-293]
 Glutathione Conjugation Support
Glutathione Conjugation Support
Glutathione is a tripeptide amino acid that depends upon adequate levels of essential nutrients such as B6, riboflavin, choline, methionine, cysteine or n-acetyl-cysteine (NAC), vitamin C, betaine, glycine, glutamic acid, potassium, copper, zinc, and selenium. Numerous studies have shown that taking these essential nutrients will enhance glutathione levels. [294,295]
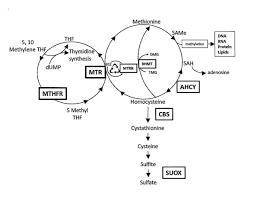 Methylation Conjugation Support
Methylation Conjugation Support
Methylation involves conjugating phase I end-products with single-carbon compounds. Methylation requires methionine, betaine, ascorbic acid, alpha tocopherol (vitamin E), choline, pyradoxyl-5-phosphate (vitamin B6), trimethlyglycine, magnesium, methylcobalamin (vitamin B12), and folic acid.
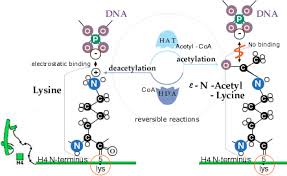 Acetylation Conjugation Support
Acetylation Conjugation Support
Acetylation pathways conjugate toxins with acetyl-CoA and two carbon compounds. Acetylation pathways are dependent on pantothenic acid, thiamin, and vitamin C.[296]
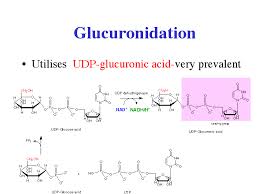 Glucuronidation Conjugation Support
Glucuronidation Conjugation Support
Glucuronidation involves combining toxins and end-products with glucuronic acid. This pathway is supported by B-vitamins, magnesium, and glycine, which help support the uronic acid pathway that synthesizes glucuronic acid.
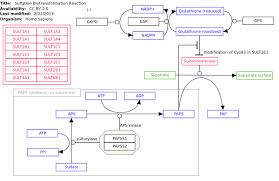 Sulfation Conjugation Support
Sulfation Conjugation Support
Sulfation involves combining toxins and end products with sulfur-containing amino acids. An important step in sulfation is the conversion of sulfites to sulfates by the molybdenum-dependent enzyme sulfite oxidase. Therefore, the mineral molybdenum and the sulfur-containing amino acids such as N-acetyl-cysteine, glycine, and methionine are important for sulfation conjugation support.
 Heavy Metal Exposure and Elimination
Heavy Metal Exposure and Elimination
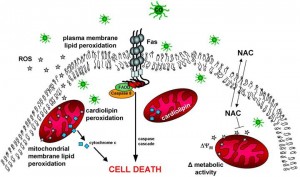
Heavy metals are eliminated by the body via different mechanisms, which rely heavily on our body’s metallothionein and glutathione systems. Metal binding proteins, including metallothioneins, are potent chelators for heavy metals and are central to the natural response of the body to these toxic elements.[297-299] Glutathione is another potent chelator involved in cellular response, transport, and excretion of metals and is a biomarker for toxic metal overload. [300-303] But it is a type of chelator that does not redistribute to other tissues, which is a big risk in many chelation therapies.[304-308] Natural compounds such as N-acetyl L-cysteine, alpha lipoic acid and glutathione all contribute to chelation and excretion of metals in the human body with much less risk of displacement into other tissues, such as the brain, than synthetic chelating agents.[309,310]
 These compounds also serve as antioxidants in the tissue to protect the tissue from damage caused by interaction with heavy metals.[311-313] Oxidative stress may be considered as one of the prime contributing mechanisms in metal toxicity and thus provide a strong rationale for including antioxidants during chelation therapy.[314] Antioxidant supplementation with chelating agents has been found beneficial in increasing metal mobilization and providing improved recovery from problems associated with chelation therapy [315-317]. Combination therapies with antioxidants like N-acetylcysteine (NAC), alpha-lipoic acid (ALA), and melatonin have shown considerable promise in improving clinical recoveries in animal models.[318] Antioxidant therapy should be considered and utilized in any protocol to support elimination of heavy metals.
These compounds also serve as antioxidants in the tissue to protect the tissue from damage caused by interaction with heavy metals.[311-313] Oxidative stress may be considered as one of the prime contributing mechanisms in metal toxicity and thus provide a strong rationale for including antioxidants during chelation therapy.[314] Antioxidant supplementation with chelating agents has been found beneficial in increasing metal mobilization and providing improved recovery from problems associated with chelation therapy [315-317]. Combination therapies with antioxidants like N-acetylcysteine (NAC), alpha-lipoic acid (ALA), and melatonin have shown considerable promise in improving clinical recoveries in animal models.[318] Antioxidant therapy should be considered and utilized in any protocol to support elimination of heavy metals.
References
47. American Autoimmune Related Diseases Association: www.aarda.com
48. Powell JJ, Van de Water J, Gershwin ME. Evidence for the role of environmental agents in the initiation or the progression of autoimmune conditions. Environ Health Perspect. 1999 Oct;107 Suppl 5:667-672
49. Yoshida S, Gershwin ME. Autoimmunity and selected environmental factors of disease induction. Semin Arthritis Rheum. 1993 Jun;22(6):399-419
50. Yoshida S, Gershwin ME. Autoimmunity and selected environmental factors of disease induction. Semin Arthritis Rheum. 1993 Jun;22(6):399-419
51. Powell JJ, Van de Water J, Gershwin ME. Evidence for the role of environmental agents in the initiation or the progression of autoimmune conditions. Environ Health Perspect. 1999 Oct;107 Suppl 5:667-672
52. Odom RY, Dansby MY, Rollins-Hairston AM, Jackson KM, Kirlin WG. Phytochemical induction of cell cycle arrest by glutathione oxidation and reversal by N-acetylcysteine in human colon carcinoma cells. Nutr Cancer. 2009;61(3):332-9.
53. Soghier LM, Brion LP. Cysteine, cystine or N-acetylcysteine supplementation in parenterally fed neonates. Cochrane Database Syst Rev. 2006 Oct 18;(4):CD004869.
54. Badaloo A, Reid M, Forrester T, Heird WC, Jahoor F. Cysteine supplementation improves the erythrocyte glutathione synthesis rate in children with severe edematous malnutrition. Am J Clin Nutr. 2002 Sep;76(3):646-52.
55. Drager LF, Andrade L, Barros de Toledo JF, Laurindo FR, Machado Cesar LA, Seguro AC. Renal effects of N-acetylcysteine in patients at risk for contrast nephropathy: decrease in oxidant stress-mediated renal tubular injury. Nephrol Dial Transplant2004;19:1803-1807.
56. Shimada K, Murayama T, Yokode M, Kita T, Uzui H, Ueda T, Lee JD, Kishimoto C. N-acetylcysteine reduces the severity of atherosclerosis in apolipoprotein E-deficient mice by reducing superoxide production. Circ J 2009;73:1337-1341.
57. Moldeus P, Cotgreave IA, Berggren M. Lung protection by a thiol-containing antioxidant: N-acetylcysteine. Respiration 1986;50 Suppl 1:31-42.
58. Prescott LF, Park J, Ballantyne A, Adriaenssens P, Proudfoot AT. Treatment of paracetamol (acetaminophen) poisoning with N-acetylcysteine. Lancet 1977;2:432-434.
59. Shay KP, Moreau RF, Smith EJ, Smith AR, Hagen TM. Alpha-lipoic acid as adietary supplement: molecular mechanisms and therapeutic potential. Biochim Biophys Acta. 2009 Oct;1790(10):1149-60. Epub 2009 Aug 4.
60. Kinnunen S, Oksala N, Hyyppä S, Sen CK, Radak Z, Laaksonen DE, Szabó B, Jakus J, Atalay M. Alpha-Lipoic acid modulates thiol antioxidant defenses and attenuates exercise-induced oxidative stress in standardbred trotters. Free Radic Res. 2009 Aug;43(8):697-705.
61. Maczurek A, Hager K, Kenklies M, Sharman M, Martins R, Engel J, Carlson DA, Münch G.Lipoic acid as an anti-infl ammatory and neuroprotective treatment for Alzheimer’s disease. Adv Drug Deliv Rev. 2008 Oct-Nov;60(13-14):1463-70.
62. Suh JH, Moreau R, Heath SH, Hagen TM. Dietary supplementation with (R)-alpha-lipoic acid reverses the age-related accumulation of iron and depletion of antioxidants in the rat cerebral cortex. Redox Rep. 2005;10(1):52-60.
63. Hill AS, Rogers QR, O’Neill SL, Christopher MM. Effects of dietary antioxidant supplementation before and after oral acetaminophen challenge in cats. Am J Vet Res. 2005 Feb;66(2):196-204.
64. Zicker SC, Hagen TM, Joisher N, Golder C, Joshi DK, Miller EP. Safety of long-term feeding of dl-alpha-lipoic acid and its effect on reduced glutathione:oxidized glutathione ratios in beagles. Vet Ther. 2002 Summer;3(2):167-76.
65. Jones W, Li X, Qu ZC, Perriott L, Whitesell RR, May JM. Uptake, recycling, and antioxidant actions of alpha-lipoic acid in endothelial cells. Free Radic Biol Med. 2002 Jul 1;33(1):83-93.
66. Miquel J. Can antioxidant diet supplementation protect against age-related mitochondrial damage? Ann N Y Acad Sci. 2002 Apr;959:508-16.
67. Khanna S, Atalay M, Laaksonen DE, Gul M, Roy S, Sen CK. Alpha-lipoic acid supplementation: tissue glutathione homeostasis at rest and after exercise. J Appl Physiol. 1999 Apr;86(4):1191-6.
68. Han D, Handelman G, Marcocci L, Sen CK, Roy S, Kobuchi H, Tritschler HJ, Flohé L, Packer L. Lipoic acid increases de novo synthesis of cellular glutathione by improving cystine utilization. Biofactors. 1997;6(3):321-38.
69. Kul M, Vurucu S, Demirkaya E, Tunc T, Aydinoz S, Meral C, Kesik V, Alpay F. Enteral glutamine and/or arginine supplementation have favorable effects on oxidative stress parameters in neonatal rat intestine. J Pediatr Gastroenterol Nutr. 2009 Jul;49(1):85-9.
70. Fan YP, Yu JC, Kang WM, Zhang Q. Effects of glutamine supplementation on patients undergoing abdominal surgery. Chin Med Sci J. 2009 Mar;24(1):55-
71. Todorova V, Vanderpool D, Blossom S, Nwokedi E, Hennings L, Mrak R, Klimberg VS.Oral glutamine protects against cyclophosphamide-induced cardiotoxicity in experimental rats through increase of cardiac glutathione. Nutrition. 2009 Jul-Aug;25(7-8):812-7.
72. Cruzat VF, Tirapegui J. Effects of oral supplementation with glutamine and alanyl-glutamine on glutamine, glutamate, and glutathione status in trained rats and subjected to long-duration exercise. Nutrition. 2009 Apr;25(4):428-35.
73. Kaufmann Y, Todorova VK, Luo S, Klimberg VS. Glutamine affects glutathione recycling enzymes in a DMBA-induced breast cancer model. Nutr Cancer. 2008;60(4):518-25.
74. Xue H, Sawyer MB, Field CJ, Dieleman LA, Murray D, Baracos VE. Bolus oral glutamine protects rats against CPT-11-induced diarrhea and differentially activates cytoprotective mechanisms in host intestine but not tumor. J Nutr. 2008 Apr;138(4):740-6.
75. Mok E, Constantin B, Favreau F, Neveux N, Magaud C, Delwail A, Hankard R. L-glutamine administration reduces oxidized glutathione and MAP kinase signaling in dystrophic muscle of mdx mice. Pediatr Res. 2008 Mar;63(3):268-73.
76. Kaufmann Y, Klimberg VS. Effect of glutamine on gut glutathione fractional release in the implanted tumor model. Nutr Cancer. 2007;59(2):199-206.
77. Belmonte L, Coëffi er M, Le Pessot F, Miralles-Barrachina O, Hiron M, Leplingard A, Lemeland JF, Hecketsweiler B, Daveau M, Ducrotté P, Déchelotte P. Effects of glutamine supplementation on gut barrier, glutathione content and acute phase response in malnourished rats during infl ammatory shock. World J Gastroenterol. 2007 May 28;13(20):2833-40.
78. Jackson AA, Gibson NR, Lu Y, Jahoor F. Synthesis of erythrocyte glutathione in healthy adults consuming the safe amount of dietary protein.Am J Clin Nutr.2004 Jul;80(1):101-7.
79. Melis GC, ter Wengel N, Boelens PG, van Leeuwen PA. Glutamine: recent developments in research on the clinical significance of glutamine. Curr Opin Clin Nutr Metab Care. 2004 Jan;7(1):59-70.
80. Johnson AT, Kaufmann YC, Luo S, Todorova V, Klimberg VS. Effect of glutamine on glutathione, IGF-I, and TGF-beta 1. J Surg Res. 2003 May 15;111(2):222-8.
81. Manhart N, Vierlinger K, Spittler A, Bergmeister H, Sautner T, Roth E. Oral feeding with glutamine prevents lymphocyte and glutathione depletion of Peyer’s patches in endotoxemic mice. Ann Surg. 2001 Jul;234(1):92-7.
82. Le Bricon T. Effect of glutamine supplementation on protein metabolism and glutathione in tumor-bearing rats. Clin Nutr. 1996 Aug;15(4):211.
83. Wichtel JJ, Thompson KG, Williamson NB. Serum glutathione peroxidase activity reflects short-term increases in selenium intake in goats. N Z Vet J. 1996 Aug;44(4):148-50
84. Delmas-Beauvieux MC, Peuchant E, Couchouron A, Constans J, Sergeant C, Simonoff M, Pellegrin JL, Leng B, Conri C, Clerc M. The enzymatic antioxidant system in blood and glutathione status in human immunodeficiency virus (HIV)-infected patients: effects of supplementation with selenium or beta-carotene. Am J Clin Nutr. 1996 Jul;64(1):101-7. Erratum in: Am J Clin Nutr 1996 Dec;64(6):971.
85. Winnefeld K, Schirrmeister W, Thiele R, Sperschneider H, Klinger G. Selenium and antioxidant status in various diseases. Med Klin (Munich). 1995 Jan 15;90 Suppl 1:7-9
86. Bellisola G, Perona G, Galassini S, Moschini G, Guidi GC. Plasma selenium and glutathione peroxidase activities in individuals living in the Veneto region of Italy. J Trace Elem Electrolytes Health Dis. 1993 Dec;7(4):242-4.
87. Bedwal RS, Nair N, Sharma MP, Mathur RS. Selenium–its biological perspectives. Med Hypotheses. 1993 Aug;41(2):150-9. PubMed
88. Zachara BA, Mikolajczak J, Trafi kowska U. Effect of various dietary selenium (Se) intakes on tissue Se levels and glutathione peroxidase activities in lambs. Zentralbl Veterinarmed A. 1993 May;40(4):310-8.
89. Wilke BC, Vidailhet M, Favier A, Guillemin C, Ducros V, Arnaud J, Richard MJ.Selenium, glutathione peroxidase (GSH-Px) and lipid peroxidation products before and after selenium supplementation. Clin Chim Acta. 1992 Apr 30;207(1-2):137-42.
90. Bellisola G, Galassini S, Moschini G, Poli G, Perona G, Guidi G. Selenium and glutathione peroxidase variations induced by polyunsaturated fatty acids oral supplementation in humans. Clin Chim Acta. 1992 Jan 31;205(1-2):75-85.
91. Pearson DJ, Day JP, Suarez-Mendez VJ, Miller PF, Owen S, Woodcock A. Human selenium status and glutathione peroxidase activity in northwest England. Eur J Clin Nutr. 1990 Apr;44(4):277-83.
92. Michaëlsson G, Edqvist LE. Erythrocyte glutathione peroxidase activity in acne vulgaris and the effect of selenium and vitamin E treatment. Acta Derm Venereol. 1984;64(1):9-14. PubMed PMID: 6203294.
93. Doni MG, Avventi GL, Bonadiman L, Bonaccorso G. Glutathione peroxidase, selenium, and prostaglandin synthesis in platelets. Am J Physiol. 1981 May;240(5):H800-3.
94. Hafeman DG, Sunde RA, Hoekstra WG. Effect of dietary selenium on erythrocyte and liver glutathione peroxidase in the rat. J Nutr. 1974 May;104(5):580-7.
95. Ko WS, Hsu SL, Chyau CC, Chen KC, Peng RY. Compound Cordyceps TCM-700C exhibits potent hepatoprotective capability in animal model. Fitoterapia. 2010 Jan;81(1):1-7.
96. Ji DB, Ye J, Li CL, Wang YH, Zhao J, Cai SQ. Antiaging effect of Cordyceps sinensis extract. Phytother Res. 2009 Jan;23(1):116-22.
97. Wang YH, Ye J, Li CL, Cai SQ, Ishizaki M, Katada M. [An experimental study on anti-aging action of Cordyceps extract]. Zhongguo Zhong Yao Za Zhi. 2004 Aug;29(8):773-6.
98. Liu Y, Wu C, Li C. [Anti-oxidation of Paecilomyces Sinensis (S. Pnov.)]. Zhongguo Zhong Yao Za Zhi. 1991 Apr;16(4):240-2, 256.
99. Haleagrahara N, Ponnusamy K. Neuroprotective effect of Centella asiatica extract (CAE) on experimentally induced parkinsonism in aged Sprague-Dawley rats. J Toxicol Sci.2010;35(1):41-7.
100. Shinomol GK, Ravikumar H; Muralidhara. Prophylaxis with Centella asiatica confers protection to prepubertal mice against 3-nitropropionicacid-induced oxidative stress in brain. Phytother Res. 2009 Nov 26.
101. Shinomol GK, Muralidhara. Prophylactic neuroprotective property of Centella asiatica against 3-nitropropionic acid induced oxidative stress and mitochondrial dysfunctions in brain regions of prepubertal mice. Neurotoxicology. 2008 Nov;29(6):948-57.
102. Shinomol GK, Muralidhara. Effect of Centella asiatica leaf powder on oxidative markers in brain regions of prepubertal mice in vivo and its in vitro efficacy to ameliorate 3-NPA-induced oxidative stress in mitochondria. Phytomedicine. 2008 Jun 5.
103. Flora SJ, Gupta R. Benefi cial effects of Centella asiatica aqueous extract against arsenic-induced oxidative stress and essential metal status in rats. Phytother Res. 2007 Oct;21(10):980-8.
104. Ramanathan M, Sivakumar S, Anandvijayakumar PR, Saravanababu C, Pandian PR.Neuroprotective evaluation of standardized extract of Centella asciatica in monosodium glutamate treated rats. Indian J Exp Biol. 2007 May;45(5):425-31.
105. Gupta R, Flora SJ. Effect of Centella asiatica on arsenic-induced oxidative stress and metal distribution in rats. J Appl Toxicol. 2006 May-Jun;26(3):213-22.
106. Jayashree G, Kurup Muraleedhara G, Sudarslal S, Jacob VB. Antioxidant activity of Centella asiatica on lymphoma-bearing mice. Fitoterapia. 2003 Jul;74(5):431-4.
107. Gupta YK, Veerendra Kumar MH, Srivastava AK. Effect of Centella asiatica on pentylenetetrazole-induced kindling, cognition and oxidative stress in rats.Pharmacol Biochem Behav. 2003 Feb;74(3):579-85.
108. Veerendra Kumar MH, Gupta YK. Effect of different extracts of Centella asiatica on cognition and markers of oxidative stress in rats. J Ethnopharmacol. 2002 Feb;79(2):253-60.
109. Lee MK, Kim SR, Sung SH, Lim D, Kim H, Choi H, Park HK, Je S, Ki YC. Asiatic acid derivatives protect cultured cortical neurons from glutamate-induced excitotoxicity. Res Commun Mol Pathol Pharmacol. 2000 Jul-Aug;108(1-2):75-86.
110. Shaker E, Mahmoud H, Mnaa S. Silymarin, the antioxidant component and Silybum marianum extracts prevent liver damage. Food Chem Toxicol. 2010 Mar;48(3):803-6.
111. Kidd PM. Bioavailability and activity of phytosome complexes from botanical polyphenols: the silymarin, curcumin, green tea, and grape seed extracts. Altern Med Rev. 2009 Sep;14(3):226-46.
112. Kaur G, Athar M, Alam MS. Dietary supplementation of silymarin protects against chemically induced nephrotoxicity, infl ammation and renal tumor promotionresponse. Invest New Drugs. 2009 Jul 10.
113. Lu P, Mamiya T, Lu LL, Mouri A, Zou L, Nagai T, Hiramatsu M, Ikejima T, Nabeshima T.Silibinin prevents amyloid beta peptide-induced memory impairment and oxidative stress in mice. Br J Pharmacol. 2009 Aug;157(7):1270-7.
114. Gharagozloo M, Moayedi B, Zakerinia M, Hamidi M, Karimi M, Maracy M, Amirghofran Z.Combined therapy of silymarin and desferrioxamine in patients with beta-thalassemia major: a randomized double-blind clinical trial. Fundam Clin Pharmacol. 2009 Jun;23(3):359-65.
115. Kim SH, Cheon HJ, Yun N, Oh ST, Shin E, Shim KS, Lee SM. Protective effect of a mixture of Aloe vera and Silybum marianum against carbon tetrachloride-induced acute hepatotoxicity and liver
fi brosis. J Pharmacol Sci. 2009 Jan;109(1):119-27.
116. Turgut F, Bayrak O, Catal F, Bayrak R, Atmaca AF, Koc A, Akbas A, Akcay A, Unal D.Antioxidant and protective effects of silymarin on ischemia and reperfusion injury in the kidney tissues of rats. Int Urol Nephrol. 2008;40(2):453-60.
117. Ligeret H, Brault A, Vallerand D, Haddad Y, Haddad PS. Antioxidant and mitochondrial protective effects of silibinin in cold preservation-warm reperfusion liver injury. J Ethnopharmacol. 2008 Feb 12;115(3):507-14.
118. Toklu HZ, Tunali Akbay T, Velioglu-Ogunc A, Ercan F, Gedik N, Keyer-Uysal M, Sener G.Silymarin, the antioxidant component of Silybum marianum, prevents sepsis-induced acute lung and brain injury. J Surg Res. 2008 Apr;145(2):214-22.
119. Song Z, Song M, Lee DY, Liu Y, Deaciuc IV, McClain CJ. Silymarin prevents palmitate-induced lipotoxicity in HepG2 cells: involvement of maintenance of Akt kinase activation. Basic Clin Pharmacol Toxicol. 2007 Oct;101(4):262-8.
120. Toklu HZ, Tunali-Akbay T, Erkanli G, Yüksel M, Ercan F, Sener G. Silymarin, the antioxidant component of Silybum marianum, protects against burn-induced oxidative skin injury. Burns. 2007 Nov;33(7):908-16.
121. Kiruthiga PV, Shafreen RB, Pandian SK, Arun S, Govindu S, Devi KP. Protective effect of silymarin on erythrocyte haemolysate against benzo(a)pyrene and exogenous reactive oxygen species (H2O2) induced oxidative stress. Chemosphere. 2007 Jul;68(8):1511-8.
122. Pradhan SC, Girish C. Hepatoprotective herbal drug, silymarin from experimental pharmacology to clinical medicine. Indian J Med Res. 2006 Nov;124(5):491-504.
123. Das SK, Vasudevan DM. Protective effects of silymarin, a milk thistle (Silybium marianum) derivative on ethanol-induced oxidative stress in liver. Indian J Biochem Biophys. 2006 Oct;43(5):306-11.
124. Edwards J, Grange LL, Wang M, Reyes E. Fetoprotectivity of the flavanolignan compound siliphos against ethanol-induced toxicity. Phytother Res. 2000 Nov;14(7):517-21.
125. Täger M, Dietzmann J, Thiel U, Hinrich Neumann K, Ansorge S. Restoration of the cellular thiol status of peritoneal macrophages from CAPD patients by the fl avonoids silibinin and silymarin. Free Radic Res. 2001 Feb;34(2):137-51
126. Valenzuela A, Aspillaga M, Vial S, Guerra R. Selectivity of silymarin on the increase of the glutathione content in different tissues of the rat. Planta Med. 1989 Oct;55(5):420-2.
127. Fahey JW, Talalay P. Antioxidant functions of sulforaphane: a potent inducer of Phase II detoxication enzymes. Food Chem Toxicol 1999;37:973-979.
128. Barcelo S, Gardiner JM, Gescher A, Chipman JK. CYP2E1-mediated mechanism of anti-genotoxicity of the broccoli constituent sulforaphane. Carcinogenesis1996;17:277-282.
129. Maheo K, Morel F, Langouet S, Kramer H, Le Ferrec E, Ketterer B, Guillouzo A.Inhibition of cytochromes P-450 and induction of glutathione S-transferases by sulforaphane in primary human and rat hepatocytes. Cancer Res 1997;57:3649-3652.
130. Peterson JD, Herzenberg LA, Vasquez K, Waltenbaugh C. Glutathione levels in antigen-presenting cells modulate Th1 versus Th2 response patterns. Proc Natl Acad Sci U S A. 1998 Mar 17; 95(6):3071-6.
131. Murata Y, Shimamura T, Hamuro J. The polarization of T(h)1/T(h)2 balance is dependent on the intracellular thiol redox status of macrophages due to the distinctive cytokine production. Int Immunol. 2002 Feb; 14(2):201-12.
132. Nazzareno Ballatori, Suzanne M. Krance, Sylvia Notenboom, Shujie Shi, Kim Tieu, Christine L. Hammond. Glutathione dysregulation and the etiology and progression of human diseases. Biol Chem. 2009 March; 390(3): 191–214.
133. Antiviral and immunomodulatory properties of new pro-glutathione (GSH) molecules. Curr Med Chem. 2006:13(15): 1749-55
134. Glutathione peroxidase 1 deficiency attenuates allergen-induced airway inflammation by suppressing TH2 and TH17 cell development. Antioxid Redox Signal. 2010 Jun 6.
135. Venu Lagishetty, Nancy Q. Liu, Martin Hewison. Vitamin D metabolism and innate immunity. Mol Cell Endocrinol. 2011 December 5; 347(1-2): 97–105.
136. Cynthia Aranow. Vitamin D and the Immune System. J Investig Med. 2011 August; 59(6): 881–886
137. Bansal AS, Henriquez F, Sumar N, Patel S. T helper cell subsets in arthritis and the benefits of immunomodulation by 1,25(OH)₂ vitamin D. Rheumatol Int. 2012 Apr;32(4):845-52.
138. Jot Hui Ooi, Jing Chen, Margherita T. Cantorna. Vitamin D regulation of immune function in the gut: Why do T cells have vitamin D receptors? Mol Aspects Med. 2012 February; 33(1): 77–82.
139. Diane L. Kamen, Vin Tangpricha. Vitamin D and molecular actions on the immune system: modulation of innate and autoimmunity. J Mol Med (Berl) 2010 May; 88(5): 441–450.
140. Margherita T. Cantorna. Vitamin D, Multiple Sclerosis and Inflammatory Bowel Disease.
Arch Biochem Biophys. 2012 July 1; 523(1): 103–106.
141. Sloka S, Silva C, Wang J, Yong VW. Predominance of Th2 polarization by vitamin D through a STAT6-dependent mechanism. J Neuroinflammation. 2011 May 24;8:56
142. Danny Bruce, Jot Hui Ooi, Sanhong Yu, Margherita T Cantorna. Vitamin D and host resistance to infection? Putting the cart in front of the horse. Exp Biol Med (Maywood) 2010 August; 235(8): 921–927.
143. Székely JI, Pataki Á. Effects of vitamin D on immune disorders with special regard to asthma, COPD and autoimmune diseases: a short review. Expert Rev Respir Med. 2012 Dec;6(6):683-704. Review.
144. Ozkara S, Keles E, Ilhan N, Gungor H, Kaygusuz I, Alpay HC. The relationship between Th1/Th2 balance and 1α,25-dihydroxyvitamin D₃ in patients with nasal polyposis. Eur Arch Otorhinolaryngol. 2012 Dec;269(12):2519-24.
145. Taher YA, van Esch BCAM, Hofman GA, Henricks PAJ, van Oosterhout AJ. 1α,25-Dihydroxy-vitamin D3 potentiates the beneficial effects of allergen immunotherapy in a mouse model of allergic asthma: role for IL-10 and TGF-β1.Journal of Immunology. 2008;180(8):5211–5221
146. Székely JI, Pataki Á. Effects of vitamin D on immune disorders with special regard to asthma, COPD and autoimmune diseases: a short review. Expert Rev Respir Med. 2012 Dec;6(6):683-704. Review.
147. Maalmi H, Berraïes A, Tangour E, Ammar J, Abid H, Hamzaoui K, Hamzaoui A. The impact of vitamin D deficiency on immune T cells in asthmatic children: a case-control study. J Asthma Allergy. 2012;5:11-9.
148. Yang CY, Leung PS, Adamopoulos IE, Gershwin ME. The implication of vitamin D and autoimmunity: a comprehensive review. Clin Rev Allergy Immunol. 2013 Oct;45(2):217-26.
149. Gatenby P, Lucas R, Swaminathan A. Vitamin D deficiency and risk for rheumatic diseases: an update. Curr Opin Rheumatol. 2013 Mar;25(2):184-91. Review.
150. Noyer CM, Simon D, Borczuk A, Brandt LJ, Lee MJ, Nehra V. A double-blind placebo-controlled pilot study of glutamine therapy for abnormal intestinal permeability in patients with AIDS. Am J Gastroenterol. 1998 Jun;93(6):972-5.
151. Klimberg VS, Souba WW, Dolson DJ, Salloum RM, Hautamaki RD, Plumley DA, Mendenhall WM, Bova FJ, Khan SR, Hackett RL, et al. Prophylactic glutamine protects the intestinal mucosa from radiation injury. Cancer. 1990 Jul 1;66(1):62-8.
152. Chamorro S, de Blas C, Grant G, Badiola I, Menoyo D, Carabaño R. Effect of dietary supplementation with glutamine and a combination of glutamine-arginine on intestinal health in twenty-five-day-old weaned rabbits. J Anim Sci. 2010 Jan;88(1):170-80.
153. Amasheh M, Andres S, Amasheh S, Fromm M, Schulzke JD. Barrier effects of nutritional factors. Ann N Y Acad Sci. 2009 May;1165:267-73
154. Kul M, Vurucu S, Demirkaya E, Tunc T, Aydinoz S, Meral C, Kesik V, Alpay F. Enteral glutamine and/or arginine supplementation have favorable effects on oxidative stress parameters in neonatal rat intestine. J Pediatr Gastroenterol Nutr. 2009 Jul;49(1):85-9.
155. Azuma H, Mishima S, Oda J, Homma H, Sasaki H, Hisamura M, Ohta S, Yukioka T. Enteral supplementation enriched with glutamine, fiber, and oligosaccharide prevents gut translocation in a bacterial overgrowth model. J Trauma. 2009 Jan;66(1):110-4.
156. Maes M, Leunis JC. Normalization of leaky gut in chronic fatigue syndrome (CFS) is accompanied by a clinical improvement: effects of age, duration of illness and the translocation of LPS from gram-negative bacteria. Neuro Endocrinol Lett. 2008 Dec;29(6):902-10.
157. Tian J, Hao L, Chandra P, Jones DP, Willams IR, Gewirtz AT, Ziegler TR. Dietary glutamine and oral antibiotics each improve indexes of gut barrier function in rat short bowel syndrome. Am J Physiol Gastrointest Liver Physiol. 2009 Feb;296(2):G348-55.
158. Coëffier M, Claeyssens S, Lecleire S, Leblond J, Coquard A, Bôle-Feysot C, Lavoinne A, Ducrotté P, Déchelotte P. Combined enteral infusion of glutamine, carbohydrates, and antioxidants modulates gut protein metabolism in humans. Am J Clin Nutr. 2008 Nov;88(5):1284-90.
159. Wang WW, Qiao SY, Li DF. Amino acids and gut function. Amino Acids. 2009 May;37(1):105-10. Epub 2008 Aug 1. Review. PubMed PMID:18670730.
160. Xue H, Sawyer MB, Field CJ, Dieleman LA, Murray D, Baracos VE. Bolus oral glutamine protects rats against CPT-11-induced diarrhea and differentially activates cytoprotective mechanisms in host intestine but not tumor. J Nutr. 2008 Apr;138(4):740-6.
161. Vicario M, Amat C, Rivero M, Moretó M, Pelegrí C. Dietary glutamine affects mucosal functions in rats with mild DSS-induced colitis. J Nutr. 2007 Aug;137(8):1931-7.
162. Harsha WT, Kalandarova E, McNutt P, Irwin R, Noel J. Nutritional supplementation with transforming growth factor-beta, glutamine, and short chain fatty acids minimizes methotrexate-induced injury. J Pediatr Gastroenterol Nutr. 2006 Jan;42(1):53-8.
163. Yeh CL, Hsu CS, Yeh SL, Chen WJ. Dietary glutamine supplementation modulates Th1/Th2 cytokine and interleukin-6 expressions in septic mice. Cytokine. 2005 Sep 7;31(5):329-34.
164. Basivireddy J, Jacob M, Balasubramanian KA. Oral glutamine attenuates indomethacin-induced small intestinal damage. Clin Sci (Lond). 2004 Sep;107(3):281-9.
165. Li N, Liboni K, Fang MZ, Samuelson D, Lewis P, Patel R, Neu J. Glutamine decreases lipopolysaccharide-induced intestinal inflammation in infant rats. Am J Physiol Gastrointest Liver Physiol. 2004 Jun;286(6):G914-21.
166. Zhou X, Li YX, Li N, Li JS. Glutamine enhances the gut-trophic effect of growth hormone in rat after massive small bowel resection. J Surg Res. 2001 Jul;99(1):47-52.K60 RepairviteTM
167. Li N, Li J, Li Y. [Nutritional rehabilitation for patients with extreme short bowel]. Zhonghua Wai Ke Za Zhi. 1997 Dec;35(12):707-9.
168. Gismondo MR, Drago L, Fassina MC, Vaghi I, Abbiati R, Grossi E. Immunostimulating effect of oral glutamine. Dig Dis Sci. 1998 Aug;43(8):1752-4.
169. Ameho CK, Adjei AA, Harrison EK, Takeshita K, Morioka T, Arakaki Y, Ito E, Suzuki I, Kulkarni AD, Kawajiri A, Yamamoto S. Prophylactic effect of dietary glutamine supplementation on interleukin 8 and tumour necrosis factor alpha production in trinitrobenzene sulphonic acid induced colitis. Gut. 1997 Oct;41(4):487-93.
170. Elia M, Lunn PG. The use of glutamine in the treatment of gastrointestinal disorders in man. Nutrition. 1997 Jul-Aug;13(7-8):743-7.
171. Wu G, Meier SA, Knabe DA. Dietary glutamine supplementation prevents jejunal atrophy in weaned pigs. J Nutr. 1996 Oct;126(10):2578-84.
172. Marks IN. Site-protective agents. Baillieres Clin Gastroenterol. 1988 Jul;2(3):609-20. Review.
173. Marks IN, Boyd E. Mucosal protective agents in the long-term management of gastric ulcer. Med J Aust. 1985 Feb 4;142(3):S23-5.
174. Russell RI, Morgan RJ, Nelson LM. Studies on the protective effect of deglycyrrhinised liquorice against aspirin (ASA) and ASA plus bile acidinduced gastric mucosal damage, and ASA absorption in rats. Scand J Gastroenterol Suppl. 1984;92:97-100.
175. Bennett A. Gastric mucosal formation of prostanoids and the effects of drugs.Acta Physiol Hung. 1984;64(3-4):215-7.
176. Morgan RJ, Nelson LM, Russell RI, Docherty C. The protective effect of deglycyrrhinized liquorice against aspirin and aspirin plus bile acid-induced gastric mucosal damage, and its influence on aspirin absorption in rats. J Pharm Pharmacol. 1983 Sep;35(9):605-7.
177. Glick L. Deglycyrrhizinated liquorice for peptic ulcer. Lancet. 1982 Oct 9;2(8302):817.
135. van Marle J, Aarsen PN, Lind A, van Weeren-Kramer J. Deglycyrrhizinised liquorice (DGL) and the renewal of rat stomach epithelium. Eur J Pharmacol. 1981 Jun 19;72(2-3):219-25.
178. Datla R, Rao SR, Murthy KJ. Excretion studies of nitrofurantoin and nitrofurantoin with deglycyrrhizinated liquorice. Indian J Physiol Pharmacol. 1981 Jan-Mar;25(1):59-63.
179. Rees WD, Rhodes J, Wright JE, Stamford LF, Bennett A. Effect of deglycyrrhizinated liquorice on gastric mucosal damage by aspirin. Scand J Gastroenterol. 1979;14(5):605-7.
180. Balakrishnan V, Pillai MV, Raveendran PM, Nair CS. Deglycyrrhizinated liquorice in the treatment of chronic duodenal ulcer. J Assoc Physicians India. 1978 Sep;26(9):811-4.
181. D’Imperio N, Giuliani Piccari G, Sarti F, Soffritti M, Spongano P, Benvenuti C, Dal Monte PR. Double-blind trial in duodenal and gastric ulcers. Cimetidine and deglycyrrhizinized liquorice. Acta Gastroenterol Belg. 1978 Jul-Aug;41(7-8):427-34.
182. Bardhan KD, Cumberland DC, Dixon RA, Holdsworth CD. Proceedings:Deglycyrrhizinated liquorice in gastric ulcer: a double blind controlled study. Gut. 1976 May;17(5):397.
183. Larkworthy W, Holgate PF. Deglycyrrhizinized liquorice in the treatment of chronic duodenal ulcer. A retrospective endoscopic survey of 32 patients.Practitioner. 1975 Dec;215(1290):787-92.
184. Aarsen PN. Standardization method of deglycyrrhizinized liquorice on experimental gastric ulcers in rats. Arzneimittelforschung. 1973 Sep;23(9): 1346-8.
185. Engqvist A, von Feilitzen F, Pyk E, Reichard H. Double-blind trial of deglycyrrhizinated liquorice in gastric ulcer. Gut. 1973 Sep;14(9):711-5.
186. Håkanson R, Liedberg G, Oscarson J, Rehfeld JF, Stadil F. Effect of deglycyrrhizinized liquorice on gastric acid secretion, histidine decarboxylase activity and serum gastrin level in the rat. Experientia. 1973 May 15;29(5):570-1.
187. Whiting B, Thomson TJ. Deglycyrrhizinized liquorice in duodenal ulcer. Br Med J. 1971 Oct 2;4(5778):48.
188. Feldman H, Gilat T. A trial of deglycyrrhizinated liquorice in the treatment of duodenal ulcer. Gut. 1971 Jun;12(6):449-51.
189. Andersson S, Bárány F, Caboclo JL, Mizuno T. Protective action of deglycyrrhizinized liquorice on the occurrence of stomach ulcers in pylorus-ligated rats. Scand J Gastroenterol. 1971;6(8):683-6.
190. Baldrick P. The safety of chitosan as a pharmaceutical excipient. Regul Toxicol Pharmacol. 2010 Apr;56(3):290-9.
191. Gunn-Moore DA, Shenoy CM. Oral glucosamine and the management of feline idiopathic cystitis. J Feline Med Surg. 2004 Aug;6(4):219-25.
192. Seidman EG, Bernotti S, Levy E. Nutritional modulation of gut inflammation.Nestle Nutr Workshop Ser Clin Perform Programme. 2002;7:41-61; discussion 61-5.
193. Sharma R, Schumacher U. Carbohydrate expression in the intestinal mucosa. Adv Anat Embryol Cell Biol. 2001;160:III-IX, 1-91.
194. Fawole OA, Amoo SO, Ndhlala AR, Light ME, Finnie JF, Van Staden J. Anti-inflammatory, anticholinesterase, antioxidant and phytochemical properties of medicinal plants used for pain-related ailments in South Africa. J Ethnopharmacol. 2010 Feb 3;127(2):235-41.
196. Ozsoy N, Candoken E, Akev N. Implications for degenerative disorders: Antioxidative activity, total phenols, flavonoids, ascorbic acid, betacarotene and beta-tocopherol in Aloe vera. Oxid Med Cell Longev. 2009 Apr;2(2):99-106.
197. Kigondu EV, Rukunga GM, Keriko JM, Tonui WK, Gathirwa JW, Kirira PG, Irungu B, Ingonga JM, Ndiege IO. Anti-parasitic activity and cytotoxicity of selected medicinal plants from Kenya. J Ethnopharmacol. 2009 Jun 25;123(3):504-9.
198. Chen W, Lu Z, Viljoen A, Hamman J. Intestinal drug transport enhancement by Aloe vera. Planta Med. 2009 May;75(6):587-95.
199. Pogribna M, Freeman JP, Paine D, Boudreau MD. Effect of Aloe vera whole leaf extract on short chain fatty acids production by Bacteroides fragilis, Bifidobacterium infantis and Eubacterium limosum. Lett Appl Microbiol. 2008 May;46(5):575-80.
200. Rosca-Casian O, Parvu M, Vlase L, Tamas M. Antifungal activity of Aloe vera leaves.Fitoterapia. 2007 Apr;78(3):219-22.
201. Iena IaM. [The therapeutic properties of aloe]. Lik Sprava. 1993 Feb-Mar;(2-3):142-5.
202. t’Hart LA, van den Berg AJ, Kuis L, van Dijk H, Labadie RP. An anticomplementary polysaccharide with immunological adjuvant activity from the leaf parenchyma gel of Aloe vera. Planta Med. 1989 Dec; 55(6):509-12.
203. Brossat JY, Ledeaut JY, Ralamboranto L, Rakotovao LH, Solar S, Gueguen A, Coulanges P.[Immunostimulating properties of an extract isolated from Aloe vahombe. 2. Protection in mice by fraction F1 against infections by Listeria monocytogenes, Yersinia pestis, Candida albicans and Plasmodium berghei]. Arch Inst Pasteur Madagascar. 1981;48(1):11-34.
204. Delaporte RH, Sarragiotto MH, Takemura OS, Sánchez GM, Filho BP, Nakamura CV.Evaluation of the antioedematogenic, free radical scavenging and antimicrobial activities of aerial parts of Tillandsiastreptocarpa Baker-Bromeliaceae. J Ethnopharmacol. 2004 Dec;95(2-3):229-33.
205. de Queiroga MA, de Andrade LM, Florêncio KC, de Fátima Agra M, da Silva MS, Barbosa-Filho JM, da-Cunha EV. Chemical constituents from Tillandsia recurvata. Fitoterapia. 2004 Jun;75(3-4):423-5.
206. Arslanian RL, Stermitz FR, Castedo L. 3-Methoxy-5-hydroxyflavonols from Tillandsia purpurea. J Nat Prod. 1986 Nov-Dec;49(6):1177-8.
207. FEURT SD, FOX LE. Effects of oral administration of Spanish moss, Tillandsia usneoides L. Science. 1953 Nov 20;118(3073):626-7.
208. FEURT SD, FOX LE. The pharmacological activity of substances extracted from Spanish moss, Tillandsia usneoides L. J Am Pharm Assoc Am Pharm Assoc (Baltim). 1952 Aug;41(8):453-4.
209. WEBBER MG, LAUTER WM, FOOTE PA. A preliminary phytochemical study of Tillandsia usneoides L. (Spanish moss). J Am Pharm Assoc Am Pharm Assoc. 1952 May;41(5):230-5.
210. Hage-Sleiman R, Mroueh M, Daher CF. Pharmacological evaluation of aqueous extract of Althaea officinalis flower grown in Lebanon. Pharm Biol. 2011 Mar;49(3):327-33.
211. Deters A, Zippel J, Hellenbrand N, Pappai D, Possemeyer C, Hensel A. Aqueous extracts and polysaccharides from Marshmallow roots (Althea officinalis L.): cellular internalisation and stimulation of cell physiology of human epithelial cells in vitro. J Ethnopharmacol. 2010 Jan 8;127(1):62-9.
212. Kardosová A, Machová E. Antioxidant activity of medicinal plant polysaccharides. Fitoterapia. 2006 Jul;77(5):367-73. Epub 2006 May 24.
213. Wang DF, Shang JY, Yu QH. [Analgesic and anti-inflammatory effects of the flower of Althaea rosea (L.) Cav.]. Zhongguo Zhong Yao Za Zhi. 1989 Jan;14(1):46-8, 64.
214. Iauk L, Lo Bue AM, Milazzo I, Rapisarda A, Blandino G. Antibacterial activity of medicinal plant extracts against periodontopathic bacteria. Phytother Res. 2003 Jun;17(6):599-604.
215. Satia JA, Littman A, Slatore CG, Galanko JA, White E. Associations of herbal and specialty supplements with lung and colorectal cancer risk in the VITamins and Lifestyle study. Cancer Epidemiol Biomarkers Prev. 2009 May;18(5):1419-28.
216. Marañón G, Muñoz-Escassi B, Manley W, García C, Cayado P, de la Muela MS, Olábarri B, León R, Vara E. The effect of methyl sulphonyl methane supplementation on biomarkers of oxidative stress in sport horses following jumping exercise. Acta Vet Scand. 2008 Nov 7;50:45.
217. Brien S, Prescott P, Bashir N, Lewith H, Lewith G. Systematic review of the nutritional supplements dimethyl sulfoxide (DMSO) and methylsulfonylmethane (MSM)in the treatment of osteoarthritis. Osteoarthritis Cartilage. 2008 Nov;16(11):1277-88.
218. Parcell S. Sulfur in human nutrition and applications in medicine. Altern Med Rev. 2002 Feb;7(1):22-44.
219. Maoka T, Tanimoto F, Sano M, Tsurukawa K, Tsuno T, Tsujiwaki S, Ishimaru K, Takii K.Effects of dietary supplementation of ferulic acid and gammaoryzanol on integument color and suppression of oxidative stress in cultured red sea bream, Pagrus major. J Oleo Sci. 2008;57(2):133-7.
220. Accinni R, Rosina M, Bamonti F, Della Noce C, Tonini A, Bernacchi F, Campolo J, Caruso R, Novembrino C, Ghersi L, Lonati S, Grossi S, Ippolito S, Lorenzano E, Ciani A, Gorini M.Effects of combined dietary supplementation on oxidative and inflammatory status in dyslipidemic subjects. Nutr Metab Cardiovasc Dis. 2006 Mar;16(2):121-7.
221. Sierra S, Lara-Villoslada F, Olivares M, Jiménez J, Boza J, Xaus J. Increased immune response in mice consuming rice bran oil. Eur J Nutr. 2005 Dec;44(8):509-16.
222. Jariwalla RJ. Rice-bran products: phytonutrients with potential applications in preventive and clinical medicine. Drugs Exp Clin Res. 2001;27(1):17-26.
223. Sugano M, Tsuji E. Rice bran oil and human health. Biomed Environ Sci. 1996 Sep;9(2-3):242-6.
224. Hirose M, Ozaki K, Takaba K, Fukushima S, Shirai T, Ito N. Modifying effects of the naturally occurring antioxidants gamma-oryzanol, phytic acid, tannic acid and n-tritriacontane-16, 18-dione in a rat wide-spectrum organ carcinogenesis model.Carcinogenesis. 1991 Oct;12(10):1917-21.
225. Wheeler KB, Garleb KA. Gamma oryzanol-plant sterol supplementation: metabolic, endocrine, and physiologic effects. Int J Sport Nutr. 1991 Jun;1(2):170-7.
226. Itaya K, Kitonaga J, Ishikawa M. [Studies of gamma-oryzanol. (2) The antiulcerogenic action]. Nippon Yakurigaku Zasshi. 1976 Nov;72(8):1001-11.
227. Brown AC, Hairfield M, Richards DG, McMillin DL, Mein EA, Nelson CD. Medical nutrition therapy as a potential complementary treatment for psoriasis-five case reports. Altern Med Rev. 2004 Sep;9(3):297-307.
228. Choi HR, Choi JS, Han YN, Bae SJ, Chung HY. Peroxynitrite scavenging activity of herb extracts. Phytother Res. 2002 Jun;16(4):364-7.
229. Majchrowicz MA. Essiac. Notes Undergr. 1995 Winter;(no 29):6-7.
230. Gill RE, Hirst EL, Jones JK. Constitution of the mucilage from the bark of Ulmus fulva (slippery elm mucilage); the sugars formed in the hydrolysis of the methylated mucilage. J Chem Soc. 1946 Nov:1025-9.
231. Jarrahi M, Vafaei AA, Taherian AA, Miladi H, Rashidi Pour A. Evaluation of topical Matricaria chamomilla extract activity on linear incisional wound healing in albino rats. Nat Prod Res. 2010 May;24(8):697-702.
232. Bezerra SB, Leal LK, Pinto NA, Campos AR. Bisabolol-induced gastroprotection against acute gastric lesions: role of prostaglandins, nitric oxide, and KATP+ channels. J Med Food. 2009 Dec;12(6):1403-6.
233. Moura Rocha NF, Venâncio ET, Moura BA, Gomes Silva MI, Aquino Neto MR, Vasconcelos Rios ER, de Sousa DP, Mendes Vasconcelos SM, de França Fonteles MM, de Sousa FC. Gastroprotection of (-)-alphabisabolol on acute gastric mucosal lesions in mice: the possible involved pharmacological mechanisms. Fundam Clin Pharmacol. 2009 Aug 3.
234. Pereira RP, Fachinetto R, de Souza Prestes A, Puntel RL, Santos da Silva GN, Heinzmann BM, Boschetti TK, Athayde ML, Bürger ME, Morel AF, Morsch VM, Rocha JB. Antioxidant effects of different extracts from Melissa officinalis, Matricaria recutita and Cymbopogon citratus. Neurochem Res. 2009 May;34(5):973-83.
235. Nogueira JC, Diniz Mde F, Lima EO. In vitro antimicrobial activity of plants in Acute Otitis Externa. Braz J Otorhinolaryngol. 2008 Jan-Feb;74(1):118-24.
236. Shikov AN, Pozharitskaya ON, Makarov VG, Kvetnaya AS. Antibacterial activity of Chamomilla recutita oil extract against Helicobacter pylori. Phytother Res. 2008 Feb;22(2):252-3.
237. Capasso R, Savino F, Capasso F. Effects of the herbal formulation ColiMil on upper gastrointestinal transit in mice in vivo. Phytother Res. 2007 Oct;21(10):999-1101.
238. Mahady GB, Pendland SL, Stoia A, Hamill FA, Fabricant D, Dietz BM, Chadwick LR. In vitro susceptibility of Helicobacter pylori to botanical extracts used traditionally for the treatment of gastrointestinal disorders. Phytother Res. 2005 Nov;19(11):988-91.
239. Madisch A, Holtmann G, Mayr G, Vinson B, Hotz J. Treatment of functional dyspepsia with a herbal preparation. A double-blind, randomized, placebo-controlled, multicenter trial. Digestion. 2004;69(1):45-52.
240. Elango G, Rahuman AA, Kamaraj C, Zahir AA, Bagavan A. Studies on effects of indigenous plant extracts on filarial vector Culex tritaeniorhynchus Giles.Parasitol Res. 2010 Apr 7.
241. Aguilar HH, de Gives PM, Sánchez DO, Arellano ME, Hernández EL, Aroche UL, Valladares-Cisneros G. In vitro nematocidal activity of plant extracts of Mexican flora against Haemonchus contortus fourth larval stage. Ann N Y Acad Sci. 2008 Dec;1149:158-60.
242. Bashir S, Gilani AH. Studies on the antioxidant and analgesic activities of Aztec marigold (Tagetes erecta) flowers. Phytother Res. 2008 Dec;22(12):1692-4.
243. Wang M, Tsao R, Zhang S, Dong Z, Yang R, Gong J, Pei Y. Antioxidant activity, mutagenicity/ anti-mutagenicity, and clastogenicity/anticlastogenicity of lutein from marigold flowers. Food Chem Toxicol. 2006 Sep;44(9):1522-9.
244. Wang M, Tsao R, Zhang S, Dong Z, Yang R, Gong J, Pei Y. Antioxidant activity, mutagenicity/anti-mutagenicity, and clastogenicity/anticlastogenicity of lutein from marigold flowers. Food Chem Toxicol. 2006 Sep;44(9):1522-9.
245. Breithaupt DE, Bamedi A, Wirt U. Carotenol fatty acid esters: easy substrates for digestive enzymes? Comp Biochem Physiol B Biochem Mol Biol. 2002 Aug;132(4):721-8.
246. Garg SC, Dengre SL. Antibacterial activity of essential oil of Tagetes erecta Linn. Hindustan Antibiot Bull. 1986 Feb-Nov;28(1-4):27-9.
247. Martín-Venegas R, Brufau MT, Guerrero-Zamora AM, Mercier Y, Geraert PA, Ferrer R.The methionine precursor DL-2-hydroxy-(4-methylthio)butanoic acid protects intestinal epithelial barrier function. Food Chem. 2013 Dec 1;141(3):1702-9.
248. Flamant M, Aubert P, Rolli-Derkinderen M, Bourreille A, Neunlist MR, Mahé MM, Meurette G, Marteyn B, Savidge T, Galmiche JP, Sansonetti PJ, Neunlist M. Enteric glia protect against Shigella flexneri invasion in intestinal epithelial cells: a role for S-nitrosoglutathione. Gut. 2011 Apr;60(4):473-84.
249. van Ampting MT, Schonewille AJ, Vink C, Brummer RJ, van der Meer R, Bovee-Oudenhoven IM. Intestinal barrier function in response to abundant or depleted mucosal glutathione in Salmonella-infected rats. BMC Physiol. 2009 Apr 17:9:6
250. Maeda T, Miyazono Y, Ito K, Hamada K, Sekine S, Horie T. Oxidative stress and enhanced paracellular permeability in the small intestine of methotrexate treated rats. Cancer Chemother Pharmacol.2010 May;65(6):1117-2
251. Savidge TC, Newman P, Pothoulakis C, Ruhl A, Neunlist M, Bourreille A, Hurst R, Sofroniew MV. Enteric glia regulate intestinal barrier function and inflammation via release of S-nitrosoglutathione. Gastroenterology. 2007 Apr;132(4):1344-1358
252. The role of the glutathione antioxidant system in gut barrier failure in a rodent model of experimental necrotizing enterocolitis. Surgery. 2004 Sep;136(3):557-66
253. Mahmood A, FitzGerald AJ, Marchbank T, Ntatsaki E, Murray D, Ghosh S, Playford RJ. Zinc carnosine, a health food supplement that stabilises small bowel integrity and stimulates gut repair processes. Gut. 2007 Feb;56(2):168-75. Epub 2006 Jun 15.
254. Kong J, Zhang Z, Musch MW, Ning G, Sun J, Hart J, Bissonnette M, Li YC. Novel role of the vitamin D receptor in maintaining the integrity of the intestinal mucosal barrier. Am J Physiol Gastroint. Liver Physiol. 2008 Jan; 294(1):G208-16
255. Vassallo MF, Camargo CA Jr. Potential mechanisms for the hypothesized link between sunshine, vitamin D, and food allergy in children. J Allergy Clin Immunol. 2010 Aug;126 (2):217-22
256. Zhao H, Zhang H, Wu H, Li H, Liu L, Guo J, Li C, Shih DQ, Zhang X. Protective role of 1,25(OH)2 vitamin D3 in the mucosal injury and epithelial barrier disruption in DSS-induced acute colitis in mice. BMC Gastroenterol. 2012 May 30;12:57.
257. Curcumin has bright prospects for the treatment of multiple sclerosis. Int Immunopharmacol. 2011 Mar;11(3):323-330
258. Curcumin, an atoxic antioxidant and natural NFkappaB, cyclooxygenase-2, lipooxygenase, and inducible nitric oxide synthase inhibitor: a shield against acute and chronic diseases. Bengmark S. JPEN J Parenter Enteral Nutr. 2006 Jan-Feb;30(1):45-51. Review.
259. Curcumin, an active component of turmeric in the prevention and treatment of ulcerative colitis: preclinical and clinical observations. Baliga MS, Joseph N, Venkataranganna MV, Saxena A, Ponemone V, Fayad R. Food Funct. 2012 Nov;3(11):1109-17. doi: 10.1039/c2fo30097d. Review.
260. Curcumin ameliorates cardiac inflammation in rats with autoimmune myocarditis. Biol Pharm Bull. 2011;34(7):974-979 JPEN J Parenter Enteral Nutr. 2006 Jan-Feb;30(1):45-51. Review.
261. “Spicing up” of the immune system by curcumin. Jagetia GC, Aggarwal BB. J Clin Immunol. 2007 Jan;27(1):19-35. Epub 2007 Jan 9. Review.
262. The targets of curcumin. Curr Drug Targets. 2011 Mar 1;12(3):332-347.
263. Oral resveratrol reduces neuronal damage in a model of multiple sclerosis. J neuroopthalmol. 2010 Dec;30(4):328-339
264. NF-kB inhibitory action of resveratrol: a probable mechanism of neuroprotection in experimental diabetic neuropathy. Biochem Biophys Res Commun. 2010 Apr 2;394(2):360-365
265. Resveratrol suppresses IL-1β-induced inflammatory signaling and apoptosis in human articular chondrocytes: potential use for use as a novel nutraceutical for the treatment of osteoarthritis. Biochem Pharmacol. 2008 Dec 1;76(11):1426-39
266. Resveratrol ameliorates experimental autoimmune myocarditis. Circ J. 2007 Mar;71(3):397-404
267. Youn J, Lee JS, Na HK, Kundu JK, Surh YJ. Resveratrol and piceatannol inhibit iNOS expression and NF-kappaB activation in dextran sulfate sodium-induced mouse colitis. Nutrition and Cancer. 2009;61(6):847–854.
268. Li T, Fan G-X, Wei W, Li T, Yuan Y-K. Resveratrol induces apoptosis, influences IL-6 and exerts immunomodulatory effect on mouse lymphocytic leukemia both in vitro and in vivo. International Immunopharmacology. 2007;7:1221–1231.
269. Oral resveratrol reduces neuronal damage in a model of multiple sclerosis. J neuroopthalmol. 2010 Dec;30(4):328-339
270. NF-kB inhibitory action of resveratrol: a probable mechanism of neuroprotection in experimental diabetic neuropathy. Biochem Biophys Res Commun. 2010 Apr 2;394(2):360-365
271. Resveratrol suppresses IL-1β-induced inflammatory signaling and apoptosis in human articular chondrocytes: potential use for use as a novel nutraceutical for the treatment of osteoarthritis. Biochem Pharmacol. 2008 Dec 1;76(11):1426-39
272. Resveratrol ameliorates experimental autoimmune myocarditis. Circ J. 2007 Mar;71(3):397-404
273. Gonzales AM, Orlando RA. Curcumin and resveratrol inhibit nuclear factor-kappaB-mediated cytokine expression in adipocytes. Nutrition and Metabolism. 2008;5(1):17–30.
274. Faber K. The dandelion Taraxacum officinale. Pharmaize 1958;13:423-436.
275. Susnik F. Present state of knowledge of the medicinal plant Taraxacum officinale. Weber. Med Razgledi 1982;21:323-328.
276. Bohm K. Choleretic action of some medicinal plants. Arzneimittel Forsch 1959;9:376-378.
277. Nassauto G et al. Effects of silbinion on biliary lipid composition. Experimental and clinical study. J Hepatol 1991;12:290-295.
278. Wagnar H. Antihepatotoxic flavonioids. In: CodyV, Middleton E, Harbourne JB, eds. Plant flavonoids in biology and medicine: biochemical, pharmacological, and structure-activity relationships. New York, NY: Alan R Liss. 1986:p545-558
279. Adzet T. Polyphenolic compounds with biological activity and pharmacological activity. Herbs Spices Medicinal Plants 1986;1:167-184
280. Hikino H, Kiso Y, Wagner H. Antihepatotoxic actions of flavanolignans from Silybum marianum fruits. Plant Medica 1984;50:248-250.
281. Fiebrich F, Koch H. Siymarin, an inhibitor of prostaglandin synthetase. Experentia 1979;35:150-152.
282. Feibrich F, Koch H. Silymarin an inbitor of lipoxygenase. Experentia 1979;35:148-150.
283. Palasciano G, Protinacasa P, et al. The effect of silymarin on plasma levels of malonadialdehyde in patients receiving long-term treatment of psychotropic drugs. Curr Ther Res 1994;55:537-545.
284. Sonnenbicher J, Goldberg M, Hane L, et al. Stimulatory effect of silibinin on the DNA synthesis in partially hepatectomized rat livers. Non-responsive in hepatoma and other malignant cel lines. Biochem
Pharm 1986;35:538-541.
285. Darnis F, Orcel L, de Saint-Maur PP, Mamaou P. Use of a titrated extract of Centella asiatica in chronic hepatic disorders. Sem Hosp Paris 1979;55:1749-1750.
286. El Zawahry MD, Kahil AM, El Banna MH. Madecassol. A new therapy for hepatic fibrosis. Bull Soc Int Chir (Belgium) 1975;34:296-297.
287. Belcaro GV, Grimaldi R, Guidi G. Improvement of capillary permeability in patients with venous hypertension after treatment with TTFCA. Angiology 1990; 41(7):533-540.
288. Pointel JP, Boccalon H, Cloarec M, et al. Titrated extract of Centella asiatca (TECA) in the treatment of venous insufficiency of the lower limbs. Angiology 1987;38(11):46-50.
289. Hikino H, Kiso Y, Sandah S, Shoji J. Antihepatotoxic actions of ginesenosides form Panax ginseng roots. Planta Medica 1985;52: 62-64.
290. Yammato M, Uemura T, Nakama S, et al. Serum HDL-cholesterol-increasing and fatty liver-improving action of Panax ginseng in high cholesterol diet-feed rats with clinical effects on hyperlipidemia in man. Am J Chin Med 1983;11:96-101.
291. Bombardelli E, Cirstoni A, Lietta A. The effect of acute and chronic (Panax) ginseng saponins treatment on adrenal function; biochemical and pharmacological. Proceedings 3rd International Ginseng Symposium.Seoul: Korean Research Institute. 1980: p 9-16.
292. Oura H, Hiai S, Seno H. Synthesis and characterization of nuclear RNA induced b Radix ginseng extract in rat liver. Chem Pharm Bull 1971;19:1598-1605.
293. Oura H, Hiai S, Nabatini S, Nakagawa H, et al. Effect of ginseng o endoplasmic reticulum and ribosome. Planta Medica 1975;28:76-88.
294. Johnston CJ, Meyer CG, Srilakshmi JC. Vitamin C elevates red blood cell glutathione levels in healthy adults. Am J Clin Nutr 1993; 58: 103-105.
295. Jain A, Buist NR, Keenaaway NG, et al. Effect of ascorbate or N-acetlycysteine treatments in patient with hereditary glutathione synthetase deficiency. J Pediatr 1994; 124: 229-233.
296. Skvortsova RI, Pzniakovski VM, Agarkova IA. Role of vitamin factor in preventing phenol poisoning. Vopr Pitan 1981; 2: 32-35.
297. Margaret E. Sears. Chelation: Harnessing and Enhancing Heavy Metal Detoxification—A Review. ScientificWorldJournal. 2013; 2013: 219840. Published online 2013 April 18. doi: 10.1155/2013/219840
298. Lynes MA, Kang YJ, Sensi SL, Perdrizet GA, Hightower LE. Heavy metal ions in normal physiology, toxic stress, and cytoprotection. Annals of the New York Academy of Sciences. 2007;1113:159–172.[PubMed]
299. Klaassen CD, Liu J, Diwan BA. Metallothionein protection of cadmium toxicity. Toxicology and Applied Pharmacology. 2009;238(3):215–220. [PMC free article] [PubMed]
300. Margaret E. Sears. Chelation: Harnessing and Enhancing Heavy Metal Detoxification—A Review. ScientificWorldJournal. 2013; 2013: 219840. Published online 2013 April 18. doi: 10.1155/2013/219840
301. Wang G, Fowler BA. Roles of biomarkers in evaluating interactions among mixtures of lead, cadmium and arsenic. Toxicology and Applied Pharmacology. 2008;233(1):92–99. [PubMed]
302. Franco R, Sánchez-Olea R, Reyes-Reyes EM, Panayiotidis MI. Environmental toxicity, oxidative stress and apoptosis: Ménage à Trois. Mutation Research/Genetic Toxicology and Environmental Mutagenesis.2009;674:3–22. [PubMed]
303. Geier DA, Kern JK, Garver CR, et al. Biomarkers of environmental toxicity and susceptibility in autism. Journal of the Neurological Sciences. 2009;280(1):101–108. [PubMed]
304. Anderson O. Chemical and biological considerations in the treatment of metal intoxications by chelating agents. Mini Rev Med Chem. 2004 Jan;4(1):11-21.
305. Ewan KB, Pamphlett R. Increased inorganic mercury in spinal motor neurons following chelationg agents. Neurotoxicaolgoy. 1996 Summer;17(2):343-349.
306. Ibim SE, Trotman J, Musey PI, Semafuko WE. Depletion of essential elements by calcium disodium EDTA treatment in the dog. Toxicology. 1992;73(2):229-237.
307. Flora SJ, Pachauri V. Chelation in metal intoxication. Int J Environ Res Public Health. 2010 Jul;7(7):2745-2788.
308. Aaseth J, Skaug MA, Cao Y, Andersen O. Chelation in metal intoxication-Principles and paradigms. J Trace Elem Med Biol. 2014 Oct 19. pii: S0946-672X(14)00180-1. doi: 10.1016/j.jtemb.2014.10.001. [Epub ahead of print] Review.
309. Margaret E. Sears. Chelation: Harnessing and Enhancing Heavy Metal Detoxification—A Review. ScientificWorldJournal. 2013; 2013: 219840. Published online 2013 April 18. doi: 10.1155/2013/219840
310. Flora SJ, Pachauri V. Chelation in metal intoxication. Int J Environ Res Public Health. 2010 Jul;7(7):2745-2788.
311. Flora SJ, Shrivastava R, Mittal M. Chemistry and pharmacological properties of some natural and synthetic antioxidants for heavymetal toxicity. Curr Med Chem. 2013;20(36):4540-74. Review.
312. Margaret E. Sears. Chelation: Harnessing and Enhancing Heavy Metal Detoxification—A Review
ScientificWorldJournal. 2013; 2013: 219840. Published online 2013 April 18. doi: 10.1155/2013/219840
313. Flora SJ, Pachauri V. Chelation in metal intoxication. Int J Environ Res Public Health. 2010 Jul;7(7):2745-2788.
314. Flora SJ, Pachauri V. Chelation in metal intoxication. Int J Environ Res Public Health. 2010 Jul;7(7):2745-2788.
315. Flora SJ, Pachauri V. Chelation in metal intoxication. Int J Environ Res Public Health. 2010 Jul;7(7):2745-2788.
316. Flora SJS. Nutritional components modify metal absorption, toxic response and chelation therapy. J. Nutri. Environ. Med. 2002;12:51–65.
317. Pande M, Flora SJS. Lead induced oxidative damage and its response to combined administration of α-Lipoic acid and succimers in rats. Toxicology. 2002;177:187–196. [PubMed]
318. Flora SJ, Pachauri V. Chelation in metal intoxication. Int J Environ Res Public Health. 2010 Jul;7(7):2745-2788.
