 In part 2, we learned that the same physiologic processes that drive biological aging are the same processes that lead to chronic disease, increased risk of poor quality of life and shorter lifespan. In order to slow down biological aging, we need to reduce our risk of developing chronic disease. In the next few articles in this series, we will review the major mechanisms of chronic and degenerative disease.
In part 2, we learned that the same physiologic processes that drive biological aging are the same processes that lead to chronic disease, increased risk of poor quality of life and shorter lifespan. In order to slow down biological aging, we need to reduce our risk of developing chronic disease. In the next few articles in this series, we will review the major mechanisms of chronic and degenerative disease.
 Take the Insulin Resistance Quiz: Do you suffer from any of the following?
Take the Insulin Resistance Quiz: Do you suffer from any of the following?
- Fatigue or drowsiness after eating?
- Need for coffee in the afternoon?
- Crave sweets after eating and during the day?
- Eating sweets does not relieve sugar cravings?
- Difficulty losing weight?
- Increased waist-to-hip ratio
- Frequent urination?
- Increased thirst and appetite?
If you have any of the above symptoms or signs, you probably have some degree of insulin resistance. But you’re not alone. Over 100 million Americans suffer from this condition.[1] That is about 1 of 3 adult Americans. The effects of insulin resistance are not the same in everyone but the ultimate consequences are the same: diabetes,[2] heart attack and stroke,[3] depression,[4] Alzheimer’s disease,[5] sleep apnea,[6] hormone imbalances,[7] obesity[8] and certain types of cancer[9]. Studies have shown almost all the chronic diseases related to aging are directly or indirectly caused by this condition.[10] [11]
 What is insulin resistance?
What is insulin resistance?
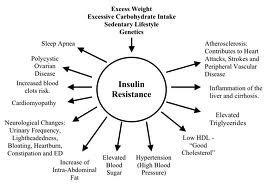
Insulin resistance is a condition that develops when we eat too much sugar or refined carbohydrates, don’t exercise, are under high amounts of stress on a regular basis and gain excess weight, especially abdominal fat. Obesity is now considered to be the largest contributor to insulin resistance.[12] No wonder why this is a national health problem! At first, our bodies are able to cope with these problems by having the pancreas produce extra insulin to lower our elevated blood sugar. But if this continues for a long period of time our bodies become resistant to the insulin being produced and the cells of the body no longer respond as efficiently to the insulin in the bloodstream. So the pancreas secretes even more insulin in order to get the same job done (lower blood sugar). This leads to hyperinsulinemia (excess insulin in the blood) and dysglycemia (blood sugar imbalances) and all the negative consequences on our health. Hyperinsulinemia and dysglycemia increase the risk of developing many chronic conditions related to aging affecting the heart, circulatory system, brain, liver, gastrointestinal tract, endocrine (hormonal) system, and the immune system as you will see.
 What are the health impacts of insulin resistance?
What are the health impacts of insulin resistance?
Excess insulin causes the following negative impacts on human physiology:
- Type 2 Diabetes
- Cardiovascular Disease
- Hormone Imbalances
- Obesity
- Impaired Liver Detoxification
- Intestinal Permeability/Leaky Gut
- Alzheimer’s Disease
- Depression
- Cancer
 Insulin Resistance and Diabetes
Insulin Resistance and Diabetes
Everyone knows that diabetes is a major health problem in the U.S. today but did you know that diabetes affects over 1.7 billion people worldwide? It is the single biggest global health epidemic of our time.[13] The prevalence of type 2 diabetes in America has tripled since the 1980s. In 2010, there were 27 million Americans with diabetes (25% of whom were not diagnosed) and 67 million with pre-diabetes (90% of whom were not diagnosed). Researchers estimate pre-diabetes will affect 1 in 2 Americans by 2020, 90% of whom will not be diagnosed. The number of diabetics is expected to increase from 1 in 10 Americans today to 1 in 3 by 2050![14]
“Obesity-induced insulin resistance is the major determinant of metabolic syndrome, which precedes the development of type 2 diabetes mellitus and is thus the driving force behind the emerging diabetes epidemic.”[15]
 Diabesity is a term used to describe the disturbance of metabolic health that results from having a problem with blood sugar balance and an excess percentage of body fat. It can range from mild to severe, depending on the stage of the disease. Mild forms of this result from having slight or no apparent blood sugar problems and being “a little” overweight. Severe forms result in full blown diabetes and obesity. The term diabesity was coined due the close relationship between diabetes and obesity.
Diabesity is a term used to describe the disturbance of metabolic health that results from having a problem with blood sugar balance and an excess percentage of body fat. It can range from mild to severe, depending on the stage of the disease. Mild forms of this result from having slight or no apparent blood sugar problems and being “a little” overweight. Severe forms result in full blown diabetes and obesity. The term diabesity was coined due the close relationship between diabetes and obesity.
Our current approach to prevention and treatment is obviously not working because millions more are affected every year. Not too long ago, this health condition was extremely rare. How does diabetes impact our health?
 Diabetes: The Leading Cause of Chronic Disease in the 21st Century
Diabetes: The Leading Cause of Chronic Disease in the 21st Century
Diabetes and its direct impact on physiology is the leading cause of most chronic disease we are now seeing in the 21st century.[16] Those with diabetes are at an increased risk of heart disease and stroke,[17] [18] [19] dementia,[20] blindness, peripheral neuropathy, kidney failure and many types of cancer.[21] [22] [23] [24] [25] [26] Diabetes is the most common cause of kidney failure. Damage to the peripheral nervous system (peripheral neuropathy) affects 75% of people with diabetes[27] and can lead to permanent nerve damage of the hands and feet, poor digestion, carpal tunnel syndrome, erectile dysfunction, and other peripheral nerve problems. Mortality rates are significantly increased in patients with type 2 diabetes.[28] So this is a very serious disease which leads to other very serious health conditions. How does diabetes impact the aging process?
 Diabetes makes you older before your time
Diabetes makes you older before your time
According to a recent study, people in their 50’s with diabetes may age before their time compared with their diabetes-free counterparts! This study showed that adults aged 51-70 with diabetes developed age-related ailments such as cognitive impairment, incontinence, falls, dizziness, vision impairment and pain at a faster rate than those without diabetes. For adults aged 51-60 with diabetes, the odds of developing new geriatric conditions were nearly double those who didn’t have diabetes!
“Because diabetes affects multiple organ systems, it has the potential to contribute significantly to the development of a number of issues that we associate with aging.”[29]
Although insulin resistance is most closely associated with the development of type 2 diabetes and its associated age-related health problems as described above, unfortunately, it doesn’t stop there. Insulin resistance also increases your risk of developing all of the following health conditions as well.
 Insulin Resistance and Cardiovascular Disease
Insulin Resistance and Cardiovascular Disease
Excess insulin itself has major impacts on cardiovascular disease. Insulin has dramatic impacts on lipid metabolism and promotes inflammation. Insulin promotes sodium retention, causing hypertension (high blood pressure).[30] Insulin resistance upregulates HMG co-reductase, which is responsible for creating cholesterol so you get higher cholesterol levels[31] and alters the activity of cholesterol ester transfer protein, causing decreased HDL (protective cholesterol).[32] This condition also leads to the inability to breakdown clotting proteins leading to increased risk of clotting and heart attack and stroke.[33] [34] Therefore, insulin resistance leads to elevated cholesterol, decreased HDL, elevated blood pressure, and increased risk of clotting. This condition is known as metabolic syndrome, also referred to as “pre-diabetes”. This condition is called a “syndrome” because it is identified by having any 3 of 5 cardiometabolic risk factors. It doesn’t meet the strict criteria for diabetes but damage occurs in the heart, circulatory system, endocrine system and brain before you get diabetes.
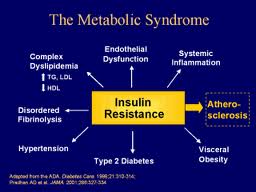 Diagnostic criteria for metabolic syndrome:
Diagnostic criteria for metabolic syndrome:
The diagnosis of metabolic syndrome is applied when 3 of the following 5 criteria are met:
- Abdominal obesity (men >40 in., women >35 in.)
- Fasting glucose >110 to 126
- BP > 130/80
- Triglycerides >150
- HDL (men <40, women <50)
 Insulin Resistance and Hormone Imbalances Elevated Testosterone in Females
Insulin Resistance and Hormone Imbalances Elevated Testosterone in Females
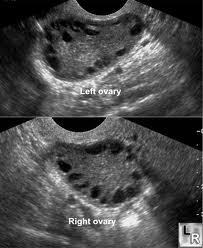
Excess insulin in females is a major driver of testosterone which leads to polycystic ovarian syndrome (PCOS).[35] Insulin upregulates an enzyme of the ovaries (17,20 lyase of the theca cells) causing increased testosterone production in females.[36] These upregulated testosterone pathways and its consequences result in polycystic ovarian syndrome (PCOS). PCOS is the #1 cause of infertility in U.S.[37] [38]
PCOS is primarily characterized by signs of excess androgens (ie: testosterone), insulin resistance and chronic anovulation (no ovulatory cycles). Symptoms range from mild to severe.
 Insulin resistance in females leads to the following symptoms:
Insulin resistance in females leads to the following symptoms:
- Irregular periods
- Infertility
- Thinning of hair and hair loss
- Growth of facial hair
- Acne
- Weight gain
- Inability to burn body fat
- Fluid retention
- Fatigue
- Mood swings
- Depression
This syndrome is also associated with estrogen proliferative cancers (ie: breast and uterine),[39] skin discoloration (acanthosis nigricans),[40] and increased cardiovascular risks.[41]
 Elevated Estrogen in Males
Elevated Estrogen in Males
In males, insulin upregulates the enzyme aromatase found in body fat, causing conversion of testosterone to estradiol. This throws off the testosterone to estradiol ratio, promoting further insulin resistance.[42] Low testosterone levels have been correlated with increased obesity, an increased waist-to-hip ratio, insulin insensitivity with higher concentrations of glucose and insulin, and increased cardiovascular risk factors including: an increase in low-density lipoproteins (LDL), a decrease in high-density lipoproteins (HDL), increased fibrinogen levels and an increase in apolipoprotein B. [43] [44] [45] [46] [47] Insulin resistance also causes increased cytokine activity (low-grade chronic inflammation) putting these men at additional risk for heart attack and other chronic diseases.[48]
“There is a common pathophysiology of insulin resistance, cytokines, and testosterone all engaged together”[49]
Insulin resistance in males leads to the following symptoms:
- low libido
- depression
- irritability and easily angered
- become emotionally sensitive
- feel warm all the time and preference for cool temperatures
- have frequent sweating attacks
 Insulin Resistance and Obesity
Insulin Resistance and Obesity
Insulin resistance plays a major role in the current obesity trends in the U.S. In insulin resistance, the cells are unable to transport glucose into the cells to be used for energy. Glucose is then forced to take an alternative pathway into lipogenesis (the creation of fats in the form of adipose tissue). This pathway is heavily dependent on ATP (your body’s primary source of fuel). This may explain why people with this condition often have fatigue after meals. There is also accumulating evidence that obesity induces insulin resistance.[50] [51] So there appears to be a “vicious cycle” that occurs between the development of obesity and insulin resistance.
Secondly, there are relationships that exist between insulin, cortisol and leptin which contribute to obesity. Leptin is a hormone produced by adipose tissue that is responsible for decreasing appetite and regulating fat storage. Insulin is an adrenal stimulant and drives up cortisol levels. This elevation of cortisol causes leptin resistance by increasing leptin to very high levels and inhibiting leptin receptors. This leads to decreased potential to burn fat and increased potential to store fat and be hungry all the time.[52] [53] [54]
 Insulin Resistance and Impaired Liver Detoxification
Insulin Resistance and Impaired Liver Detoxification
Dysglycemia and insulin resistance also leads to compromised phase I and phase II liver detoxification pathways.[55] [56] These are important pathways of the liver involved in eliminating certain drugs, toxins and hormones from the body. Insulin surges downregulate one of the enzymes (G6PD) involved in glutathione production.[57] [58] When glutathione levels are suppressed, phase I and phase II detoxification will be compromised. Glutathione is the main antioxidant for our cells and is important for both phase I and phase II pathways of detoxification. When glutathione levels drop, inflammatory processes associated with aging such as neuropathies,[59] vascular disease,[60] autoimmune disease,[61] neurodegenerative disease,[62] and many other problems develop as documented in numerous studies.[63] [64] [65] Chronic dysglycemia causes compromised liver pathways and ability to clear drugs and toxins from the body leading to symptoms associated with toxicity, such as acne, constipation, bloating and drug or chemical sensitivities.
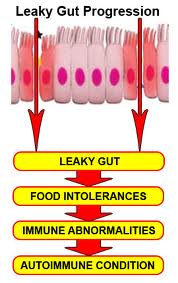 Insulin Resistance and “Leaky Gut”
Insulin Resistance and “Leaky Gut”
Elevated cortisol levels seen in insulin resistance have adverse effects on the gastrointestinal tract by suppressing secretory IgA (SIgA), delaying mucosal cell regeneration and by promoting a pro-inflammatory environment.[66] [67] [68] SIgA cells are the barrier defense cells of the gastrointestinal (GI) lining and protect against GI infection. “Leaky gut” (intestinal permeability) patterns develop when SIgA levels drop. “Leaky gut” is a condition in which the barrier of the intestinal tract becomes compromised and there is increased penetration of large molecules, such as undigested protein molecules, bacteria and toxins.[69] This leads to chronic inflammation and increased risk of autoimmune disease.[70]
“There is growing evidence that increased intestinal permeability plays a pathogenic role in various autoimmune diseases. Therefore, we hypothesize that loss of intestinal barrier function is necessary to develop autoimmunity”[71]
 Insulin Resistance and Depression, Dementia and Neurodegenerative Disease
Insulin Resistance and Depression, Dementia and Neurodegenerative Disease
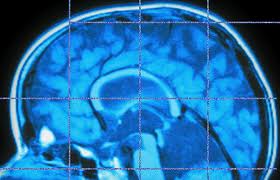
Pioneering new work out of Harvard and Brown universities from Dr. Denis Selkoe and Suzanne de la Monte has proved that insulin resistance is a major factor in starting the cascade of brain damage that steals the memory of over half of people in their eighties, leading to a diagnosis of Alzheimer’s disease. The reason is that insulin resistance leads to a cascade of damage, which produces the inflammation so characteristic of brain problems, especially dementia and depression.[72] Recent studies have shown that diabetics have a fourfold increased risk of developing Alzheimer’s disease. There is such a close association between insulin resistance of the brain and the development of Alzheimer’s disease, that this disease is now being called “type 3 diabetes”.[73]
One study of 2,632 men and women over five years recently published in JAMA found that those with metabolic syndrome and inflammation had dramatic declines in cognitive function.[74] It is called mild cognitive impairment. This is a prelude to dementia.
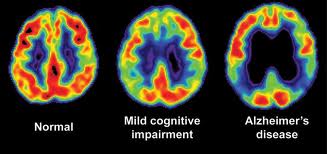 PET scans which look at brain metabolism have found altered and damaged brain function that occurs far in advance of the diagnosis of dementia.[75] Some experts say that changes can be identified decades before diagnosis. This process of decline starts in childhood and adolescence. Given the epidemic of childhood obesity and the fact that we are seeing heart disease in twenty-year-olds, we may soon see an epidemic of Alzheimer’s when these kids enter their forties and fifties.
PET scans which look at brain metabolism have found altered and damaged brain function that occurs far in advance of the diagnosis of dementia.[75] Some experts say that changes can be identified decades before diagnosis. This process of decline starts in childhood and adolescence. Given the epidemic of childhood obesity and the fact that we are seeing heart disease in twenty-year-olds, we may soon see an epidemic of Alzheimer’s when these kids enter their forties and fifties.
It is well known that depression is more common in diabetes, but a Finnish study of young men found that those who had the worst insulin resistance had an almost 3-fold risk of having severe depression.[76]
 Insulin Resistance and Cancer
Insulin Resistance and Cancer
There is increasing evidence in the literature regarding the role excess insulin plays in carcinogenesis (initiation of cancer) for various types of cancer.[77] [78] The studies are becoming more conclusive on insulin’s role in promoting inflammatory responses and its numerous adverse impacts on human metabolism.
 Insulin and Chronic Inflammation
Insulin and Chronic Inflammation
As individuals develop insulin resistance and obesity, increased inflammatory cytokines (chemical messengers/mediators) are produced.[79] [80] [81] [82] Many of these cytokines fire each other up initiating further inflammatory processes. Increased inflammation promotes increased tissue destruction and catabolic (breakdown of tissue) processes in the body and many of the chronic diseases associated with aging as we will learn in the next article. Stay tuned!
References:
[1] Grimm JJ. Interaction of physical activity and diet: implications for insulin-glucose dynamics- Public Health Nutr 1999;2:363-368.
[2] Moore MA, et al. Implications of the hyperinsulinemia -diabetes-cancer link for preventative efforts. Eur J Cancer Prev 1998;7:89-107
[3] Despres JP, et al. Hyperinsulinemia as an independent risk factor for ischemic heart disease. N Eng J Med 1996;334:952-957.
[4] Timonen, M. et al. 2007. Insulin resistance and depressive symptoms in young adult males: Findings from Finnish military conscripts. Psychosom Med 69(8):723-28
[5] Kinoshita, J.; Alzheimer Research Forum. 2006. Alzheimer Research Forum live discussion: Insulin resistance: a common axis linking Alzheimer’s, depression and metabolism? J Alzheimers Dis 9 (1):89-93
[6] Tiihonen M, Partinen M. Narvanen S. The severity of obstructive sleep apnea is associated with insulin resistance. J Sleep Res 1993;2:56-61.
[7] Arthur LS, Selvakumar R, Seshardir MS. Hyperinsulinemia in polycystic ovary disease. J Reprod Med 1999;44:783-787.
[8] Benzi L, et al. Intracellular hyperinsulinemia: a metabolic characteristic of obesity with and without type 2 diabetes: intracellular insulin in obesity and type 2 diabetes. Diabetes Res Clin Pract 1999:46:231-237.
[9] Stoll BA. Essential fatty acids, insulin resistance and breast cancer risk Nutr Cancer 1998;31:72-77.
[10] Bhashyam, S, et al. Aging is associated with myocardial insulin resistance and mitochondrial dysfunction. Am J Physiol Heart Circ Physiol. 2007 Nov;293(5):H3063-71.
[11] Ryan AS. Insulin resistance with aging: effects of diet and exercise. Sports Med. 2000 Nov;30(5):327-46. Review
[12] Johnson AM, Olefsky JM. The origins and drivers of insulin resistance. Cell. 2013 Feb 14;152(4):673-84. doi: 10.1016/j.cell.2013.01.041.
[13] Ginter E, Simko V. Type 2 diabetes mellitus, pandemic in 21st century. Adv Exp Med Biol. 2012;771:42-50.
[14] Mark Hyman. The Blood Sugar Solution; Little, Brown and Company. 2012
[15] Johnson AM, Olefsky JM. The origins and drivers of insulin resistance. Cell. 2013 Feb 14;152(4):673-84. doi: 10.1016/j.cell.2013.01.041.
[16] http://apps.nccd.cdc.gov/DDTSTRS/FactSheet.aspx (National Diabetes Fact Sheet 2007)
[17] http://www.cdc.gov/diabetes/statistics/cvd/fig5.htm
[18] Lakka HM, Laaksonen DE, Lakka TA, Niskanen LK, Kumpusalo E, Tuomilehto J, Salonen JT. The metabolic syndrome and total and cardiovascular disease mortality in middle-aged men. JAMA. 2002 Dec 4;288(21):2709-16.
[19] Kuwahara M, et al. Type II diabetes mellitus is a risk factor for heart failure in pre-dialysis patients. Ther Apher Dial. 2012 Dec;16(6):541-7. doi: 10.1111/j.1744-9987.2012.01090.x. Epub 2012 Aug 13.
[20] Ott A, Stolk RP, van Harskamp F, Pols HA, Hofman A, Breteler MM. Diabetes mellitus and the risk of dementia: The Rotterdam Study. Neurology. 1999 Dec 10;53(9):1937-42.
[21] Yoon JM, et al. Pre-existing diabetes mellitus increases the risk of gastric cancer: A meta-analysis. World J Gastroenterol. 2013 Feb 14;19(6):936-45. doi: 10.3748/wjg.v19.i6.936.
[22] Fujii M, et al. A murine model for non-alcoholic steatohepatitis showing evidence of association between diabetes and hepatocellular carcinoma. Med Mol Morphol. 2013 Feb 22. [Epub ahead of print]
[23] Bao C, et al. Diabetes mellitus and incidence and mortality of kidney cancer: A meta-analysis. J Diabetes Complications. 2013 Feb 20. pii: S1056-8727(13)00005-6. doi: 10.1016/j.jdiacomp.2013.01.004. [Epub ahead of print]
[24] Zhu Z, et al. Diabetes mellitus and risk of bladder cancer: a meta-analysis of cohort studies. PLoS One. 2013;8(2):e56662. doi: 10.1371/journal.pone.0056662. Epub 2013 Feb 20.
[25] Amudhan S, Krishnan A. Diabetes mellitus: a risk factor for cancer and non-vascular disease deaths too. Natl Med J India. 2011 Jul-Aug;24(4):222-4.
[26] Pandey A, et al. Diabetes mellitus and the risk of cancer. Minerva Endocrinol. 2011 Sep;36(3):187-209.
[27] Ugoya SO, et al. Clinically diagnosed diabetic neuropathy: frequency, types and severity. J Natl Med Assoc. 2006 Nov;98(11):1763-6.
[28] Barkoudah E et al. Mortality rates in trials of subjects with type 2 diabetes. J Am Heart Assoc. 2012 Feb;1(1):8-15. doi: 10.1161/JAHA.111.000059. Epub 2012 Feb 20.
[29] Cigolle CT et al. Geriatric conditions develop in middle-aged adults with diabetes. J Gen Intern Med. 2011 Mar;26(3):272-9. doi: 10.1007/s11606-010-1510-y. Epub 2010 Sep 29.
[30] Zavaroni I, Mazza S, Dall’aglio E, et al. Prevelance of hyperinsulinemia in patients with high blood pressure. J int Med 1992;231:235-240.
[31] Dietschy JM, Brown MS. Effect of alterations of the specific activity of the intracellular acetyl CoA pool apparent rates of hepatic cholesterogenesis. J Lipid Res 1974;15:508-516.
[32] Swensen TL. The role of cholesteryl ester transfer protein in lipoprotein metabolism. Diabetes Metab Res 1991;7:139-153.
[33] Potter van Loon, et al. The cardiovascular risk factor plasminogen activator inhibitor type I is related to insulin resistance. Metabolism 1993;42:945-949.
[34] Juhan-Vague, et al. Fibrinolytic factors and the risk of myocardial infarction or sudden death in patients with angina pectoris. Circulation 1996;94(9):2057-2063.
[35] Stepto NK, et al. Women with polycystic ovary syndrome have intrinsic insulin resistance on euglycaemic-hyperinsulaemic clamp. Hum Reprod. 2013 Mar;28(3):777-84. doi: 10.1093/humrep/des463. Epub 2013 Jan 12.
[36] Jakubowski L. Endokrynol Pol. 2005 May-Jun;56(3):285-93. Review. [Genetic aspects of polycystic ovary syndrome].
[37] Sozen I, Arici A. Hyperinsulinism and its interaction with hyperandrogenism in polycystic ovary syndrome. Obest Gynecol Surv 2000;55:321-328.
[38] Nestler J. Insulin resistance effects on sex hormones and ovulation in the polycystic ovary syndrome. In:Reaven G, Laws A, eds. Contemporary Endocrinology; Insulin Resistance. Totowa NJ: Humana Press; 1999.347-365.
[39] Dahlgreen E, et al. Women with polycystic ovary syndrome wedge resected in 1956 to 1965: a long term follow-up focusing on natural history and circulating hormones. Fertil Steril 1992;57:505-513.
[40] Oberfiled S. Metabolic lessons from the study of young adolescents with polycystic ovary syndrome, is insulin indeed the culprit. J Clin Endocrinol Metab 2000;85:3520-3525.
[41] Wild RA. Obesity, lipids, cardiovascular risk and androgen excess. Am J Med 1995;98:27S-32S.
[42] The promoters of the aromatase gene in male testicular cells. Reprod Biol. 2004 Mar;4(1):23-34
[43] Phillips GB, Pinkernall BH, Jing TY. The association of hypotestosteronemia with coronary artery disease in men. Arterioscler Thromb 1994;14:701-706
[44] Zgliczynski S, et al. Effects of testosterone replacement thereapy on lipids and lipoproteins in hypogonadic and elderly men. Atherosclerosis. 1996:121(1):35-43
[45] Chou T, et al. Testosterone induces dilation of canine coronary conductance and resistance arteries in vivo. Circulation. 1996:94(10):2614-2619
[46] Phillips G, et al. Sex hormones and hemostatic risk factors for coronary heart disease in men with hypertension. J of Hypertension. 193:11(7):699-702
[47] Jepsen L, et al. Decreased serum testosterone in men with acute ischemic stroke. Arterioscler Thromb Basc Biol, 1996:16(6):749-754
[48] Hypogonadotrophic hypogonadism in type 2 diabetes Aging Male. 2008 Sep;11(3):107-117
[49] Testosterone deficiency, insulin resistance and the metabolic syndrome. Nat Rev Endocrinol. 2009 Dec;5;(12):673-681
[50] Johnson AM, Olefsky JM. The origins and drivers of insulin resistance. Cell. 2013 Feb 14;152(4):673-84. doi: 10.1016/j.cell.2013.01.041.
[51] Galgani J, Díaz E. Rev Med Chil. 2000 Dec;128(12):1354-60. [Obesity and fatty acids in the etiology of insulin resistance].
[52] Zakrzewska KE, et al. Glucocorticoids as counterregulatory hormones of leptin: toward an understanding of leptin resistance. Diabetes 1997;46:717-719.
[53] Zakrzewska, et al. Induction of obesity and hyperleptinemia by central glucocorticoid infusion in the rat. Diabetes 1999;48:365-370.
[54] Bermeis K, Vosmeer S, Kelly U. Effects of glucocorticoids and of growth hormone on serum leptin concentrations in man. Eur J Endocrinol 1996;663-665.
[55] Vávrová L, et al. Altered Activities of Antioxidant Enzymes in Patients with Metabolic Syndrome. Obes Facts. 2013 Feb 21;6(1):39-47. [Epub ahead of print].
[56] Ozgen IT, et al. Oxidative stress in obese children and its relation with insulin resistance. J Pediatr Endocrinol Metab. 2012;25(3-4):261-6.
[57] Xu, Y, et al. Diabetes causes inhibition of glucose-6-phosphate dehydrogenase via activation of PKA, which contributes to oxidative stress in rat kidney cortex. Am J Physiol Renal Physiol. 2005 Nov;289(5):F1040-7. Epub 2005 Jun 14.
[58] Iwakiri, R, et al. Determinants of hydroperoxide detoxification in diabetic rat intestine: effect of insulin and fasting on the glutathione redox cycle. Metabolism. 1995 Nov;44(11):1462-8.
[59] Cameron NE, Cotter MA. Metabolic and vascular factors in the pathogenesis of diabetic neuropathy. Diabetes. 1997 Sep;46 Suppl 2:S31-7.
[60] Weldy CS, et al. Glutathione (GSH) and the GSH synthesis gene Gclm modulate vascular reactivity in mice. Free Radic Biol Med. 2012 Sep 15;53(6):1264-78. doi: 10.1016/j.freeradbiomed.2012.07.006. Epub 2012 Jul 21.
[61] Shah D, et al. Altered redox state and apoptosis in the pathogenesis of systemic lupus erythematosus. Immunobiology. 2012 Aug 4. [Epub ahead of print]
[62] Lee M, et al. Depletion of GSH in glial cells induces neurotoxicity: relevance to aging and degenerative neurological diseases. FASEB J. 2010 Jul;24(7):2533-45. doi: 10.1096/fj.09-149997. Epub 2010 Mar 12.
[63] Mari M, et al. Mitochondrial glutathione: Features, regulation and role in disease. Biochim Biophys Acta. 2012 Oct 30. pii: S0304-4165(12)00304-2. doi: 10.1016/j.bbagen.2012.10.018. [Epub ahead of print]
[64] Droge W and Breitkreutz R. Glutathione and immune function. Proc Nutr Soc. 2000. 59 (4):595-600. Review
[65] Faut M, et al. Alterations of the redox state, pentose pathway and glutathione metabolism in an acute porphyria model. Their impact on heme pathway. Exp Biol Med (Maywood). 2013 Feb 6. [Epub ahead of print]
[66] Guhad, FA, et al. Salivary IgA as a marker of social stress in rats. Neurosci Lett, 216(2). 137-140, 1996.
[67] Cunningham-Rundies, C., et al. Proc. Nat Acada. Sci USA. 75:3387, 1978.
[68] Cunningham-Rundies, C., et al. J Clin Invest. 64:270, 1979.
[69] Liu Z, et al. Tight junctions, leaky intestines, and pediatric diseases. Acta Paediatr. 2005 Apr;94(4):386-93.
[70] Mechanisms of disease: the role of intestinal barrier function in the pathogenesis of gastrointestinal autoimmune diseases. Nat Clin Pract Gastroenterol Hepatol. 2005 Sep;2(9): 416-22
[71] Tight junctions, intestinal permeability, and autoimmunity: celiac disease and type 1 diabetes paradigms. Ann N Y Acad Sci. 2009 May;1165:195-205
[72] Kinoshita, J.; Alzheimer Research Forum. 2006. Alzheimer Research Forum live discussion: Insulin resistance: a common axis linking Alzheimer’s, depression and metabolism? J Alzheimers Dis 9 (1):89-93
[73] De la Monte SM, Wands JR. Alzheimer’s disease is type 3 diabetes—evidence reviewed. J Diabetes Sci Technol. 2008 Nov;2(6):1101-13.
[74] Yaffe, K. et al. 2004 The metabolic syndrome, inflammation, and risk of cognitive decline. JAMA 292 (18):2237-2242.
[75] Silverman, DH, et al. 2001. Positron emission tomography in evaluation of dementia: regional brain metabolism and long-term outcome. JAMA 286(17):2120-127.
[76] Timonen, M. et al. 2007. Insulin resistance and depressive symptoms in young adult males : Findings from Finnish military conscripts. Psychosom Med 69(8):723-28
[77] Perseghin G et al. Insulin resistance/hyperinsulinemia and cancer mortality: the Cremona study at the 15th year of follow-up. Acta Diabetol. 2012 Dec;49(6):421-8. doi: 10.1007/s00592-011-0361-2. Epub 2012 Jan 4.
[78] Faulds MH, Dahlman-Wright K. Metabolic diseases and cancer risk. Curr Opin Oncol. 2012 Jan;24(1):58-61. doi: 10.1097/CCO.0b013e32834e0582.
[79] Ojeda-Ojeda M, et al. Mediators of Low-Grade Chronic Inflammation in Polycystic Ovary Syndrome (PCOS). Curr Pharm Des. 2013 Feb 20. [Epub ahead of print]
[80] Boden G, Salehi S. Why Does Obesity Increase the Risk for Cardiovascular Disease? Curr Pharm Des. 2013 Feb 20. [Epub ahead of print]
[81] Mauvais-Jarvis F. Novel link between inflammation, endothelial dysfunction, and muscle insulin resistance. Diabetes. 2013 Mar;62(3):688-90. doi: 10.2337/db12-1434.
[82] Vávrová L, et al. Altered Activities of Antioxidant Enzymes in Patients with Metabolic Syndrome. Obes Facts. 2013 Feb 21;6(1):39-47. [Epub ahead of print]