- What is your chemical load?
- Does it matter?
- Are you exposed to harmful chemicals right now?
- Are your kids being exposed?
- What can you do about it?
In this 4-segmented series of part 7, we examine the effects of common environmental chemicals and toxins on human health according to the most recent research, focusing on impacts on the immune system. In this first segment, we briefly review the increasing amounts of environmental pollutants we are exposed to on a daily basis and how they may be contributing to the escalating pandemic of allergy, immune disorders and inflammatory and neurodegenerative diseases. We examine the most important chemicals and toxins in our environment, according to the U.S. government, and review their potential health impacts according to the most recent literature available.
 In the next segment, we review the 12 most common endocrine disruptors according to the Environmental Working Group and 4 other important environmental toxins and summarize the potential health effects of these compounds according to the most recent research. We review the evidence showing how these compounds may be contributing to various hormonal and reproductive disorders, cognitive and neurological disorders, kidney and liver disease, immunological disorders and cancer. We also make recommendations on how you can protect you and your family against exposure to each of these toxic compounds.
In the next segment, we review the 12 most common endocrine disruptors according to the Environmental Working Group and 4 other important environmental toxins and summarize the potential health effects of these compounds according to the most recent research. We review the evidence showing how these compounds may be contributing to various hormonal and reproductive disorders, cognitive and neurological disorders, kidney and liver disease, immunological disorders and cancer. We also make recommendations on how you can protect you and your family against exposure to each of these toxic compounds.
 Key concepts for this issue
Key concepts for this issue
- Environmental Toxicity and Potential Impacts on Human Health
- Increasing Prevalence of Allergies and Immune-Related Disorders
- Polypharmacy in the U.S.
- The Environmental Pollutant-Neuro-Endocrine-Immune Connection
- Have These Chemicals Been Shown To Be Safe?
- Are Our Kids Being Exposed?
- Top 10 U.S. Government Priority List of Hazardous Substances
 Environmental Toxicity and Potential Impacts on Human Health
Environmental Toxicity and Potential Impacts on Human Health
We are living in a world that has changed dramatically just within our lifetimes. We are now exposed to countless chemicals, hybridized foods, genetically-modified foods, all of which are very immune-activating. There are now more than 84,000 different chemicals used in making products such as food, clothes, furniture, electronics and toys that we are potentially exposed to on a daily basis and about 1,500 new chemicals are introduced each year.[1] Environmental chemicals are linked with various cancers, obesity, diabetes, heart disease, brain degeneration, neurological disorders and almost every known health issue. But these links can be difficult to identify and the published data difficult for the average person to understand. Unless there is an acute exposure, exposure to chemical pollutants usually occurs gradually over a long period of time and effects tend to be cumulative.
 Since most people are exposed to a number of toxic chemicals simultaneously throughout their lives and the effects are cumulative, effects of specific environmental chemicals or toxins on human health are difficult for researchers to isolate. The exception to this is fetal exposure to toxins during critical periods of development, particularly during development of the brain and nervous system. As you can imagine, it is unethical to conduct human trials on the effects of toxic chemical exposure on humans, as is often done when studying the effects of pharmaceuticals, for example. Therefore, researchers tend to rely two types of studies: animal studies (often using rats or other rodents) which may be exposed to high amounts of toxins and epidemiological studies, meaning they look at populations of people in specific areas who are likely to have or are known to have had higher amounts of exposures to a specific type of chemical or toxin than the normal population. The other type of study that is being done more recently is looking at the developmental effects of chemical exposure of the pregnant mother to the developing fetus and how it impacts child development.
Since most people are exposed to a number of toxic chemicals simultaneously throughout their lives and the effects are cumulative, effects of specific environmental chemicals or toxins on human health are difficult for researchers to isolate. The exception to this is fetal exposure to toxins during critical periods of development, particularly during development of the brain and nervous system. As you can imagine, it is unethical to conduct human trials on the effects of toxic chemical exposure on humans, as is often done when studying the effects of pharmaceuticals, for example. Therefore, researchers tend to rely two types of studies: animal studies (often using rats or other rodents) which may be exposed to high amounts of toxins and epidemiological studies, meaning they look at populations of people in specific areas who are likely to have or are known to have had higher amounts of exposures to a specific type of chemical or toxin than the normal population. The other type of study that is being done more recently is looking at the developmental effects of chemical exposure of the pregnant mother to the developing fetus and how it impacts child development.
 Increasing Prevalence of Allergies and Immune-Related Disorders
Increasing Prevalence of Allergies and Immune-Related Disorders
Studies show that food allergy among children in the U.S. is becoming more common over time. During the 10-year period from 1997 to 2006, food allergy rates increased significantly among both preschool-aged and older children.[2] A more recent large-scale study showed that prevalence of food allergy was 8.0% in 2011.[3] This means that food allergies affected approximately 1 in 12 children in 2011! Among children with food allergy, over 38% had a history of severe reactions, and over 30% had multiple food allergies. The most common food allergens were: peanut (25%), followed by milk (21%) and shellfish (17%).[4] The researchers of this 2011 study concluded the following:
“Findings suggest that the prevalence and severity of childhood food allergy is greater than previously reported.”[5]
 Children with food allergy are more likely to have asthma or other allergic conditions
Children with food allergy are more likely to have asthma or other allergic conditions
Children with food allergy are two to four times more likely to have other immune-mediated related conditions such as asthma and other allergies, compared with children without food allergies. This is of great importance as children with coexisting food allergy and asthma may be more likely to experience anaphylactic reactions to foods and be at higher risk of death.[6]
Recent data also shows hospitalizations with diagnoses related to food allergies have also increased among children. Hospital discharges with a diagnosis related to food allergy increased significantly (almost 4 times) over time from 1998–2000 through 2004–2006. From 2004 to 2006, there were an average of 9,537 hospital discharges per year with a diagnosis related to food allergy among children 0 to 17 years![7]
 Dietary Impacts on Our Health
Dietary Impacts on Our Health
When we look at our diets, there are two startling trends. The first is our increasing exposure to pesticides, herbicides, antibiotics, pharmaceuticals and other chemicals and toxins in our food and water supply. The second is our increased consumption of processed foods, fast food and food no longer in a natural state. The standard American diet is not only very inflammatory but very immune-activating. Many Americans turn to fast food and processed foods on a regular basis and there are increasing amounts of genetically-modified foods (which are still not labelled as GMO in most states) and food products that are composed of very inexpensive low nutrient-dense food such as wheat and other grains which are attractive to many low-budget consumers. The focus of this article will be on the trend of increasing environmental chemical and toxic exposures and the impacts on our health.
 Polypharmacy in the U.S.
Polypharmacy in the U.S.
In addition to environmental exposures, the increased use of pharmaceutical drugs is absolutely shocking. Among the startling statistics, the United States now consumes 80% of the world’s opioid pain medications and 99% of the world’s hydrocodone (semi-synthetic opioid). The milligram per person use of prescription opioids in the United States increased 402% (more than 4 times), between 1997 and 2007.[8a] According to the Centers for Disease Control (CDC) National Center for Health Statistics’ Data Brief, the percentage of Americans who took at least one prescription drug in the past month increased from 44% to 48% over the last 10 years. The use of two or more drugs increased from 25% to 31%. The use of five or more drugs increased from 6% to 11%. In 2007-2008, 1 out of every 5 children and 9 out of 10 older Americans reported using at least one prescription drug in the past month.[8b]
 The most commonly used types of drugs included: central nervous system (brain) stimulants for children, antidepressants for middle-aged adults, and cholesterol lowering drugs for older Americans. Spending for prescription drugs in the U.S. was $234.1 billion in 2008, which was more than double what was spent in 1999.[8c] Overall, the number of Americans on medications used to treat psychological and behavioral disorders has substantially increased since 2001; more than one‐in‐five adults was on at least one of these medications in 2010, up 22 percent from ten years earlier.[8d] According to the World Health Organization, in 1999, the 15% of the world’s population who live in high-income countries (like the U.S.) purchased and consumed about 90% of total medicines, by value. The market share of the USA alone rose from 18.4% of the world total in 1976 to over 52% in 2000![8e] This means that Americans are now consuming over one-half of the medications being used worldwide, by value!
The most commonly used types of drugs included: central nervous system (brain) stimulants for children, antidepressants for middle-aged adults, and cholesterol lowering drugs for older Americans. Spending for prescription drugs in the U.S. was $234.1 billion in 2008, which was more than double what was spent in 1999.[8c] Overall, the number of Americans on medications used to treat psychological and behavioral disorders has substantially increased since 2001; more than one‐in‐five adults was on at least one of these medications in 2010, up 22 percent from ten years earlier.[8d] According to the World Health Organization, in 1999, the 15% of the world’s population who live in high-income countries (like the U.S.) purchased and consumed about 90% of total medicines, by value. The market share of the USA alone rose from 18.4% of the world total in 1976 to over 52% in 2000![8e] This means that Americans are now consuming over one-half of the medications being used worldwide, by value!
 This polypharmacy model of various drugs has potentially diverse impacts on human physiology beyond known adverse reactions. But the potentially harmful effects of medications don’t stop there. Healthy animals used for human consumption are often treated with antibiotics to prevent disease and hormones to increase growth rate which have potential consequences on the health of the consumer. Additionally, studies show that many of these pharmaceutical drugs are making their way into our tap water along with environmental heavy metals, chemicals and toxins while standards of testing of these compounds and water quality varies significantly in each municipality across the country. The totality of these environmental chemicals, pollutants and synthetic compounds are unquestionably having an impact on our health.
This polypharmacy model of various drugs has potentially diverse impacts on human physiology beyond known adverse reactions. But the potentially harmful effects of medications don’t stop there. Healthy animals used for human consumption are often treated with antibiotics to prevent disease and hormones to increase growth rate which have potential consequences on the health of the consumer. Additionally, studies show that many of these pharmaceutical drugs are making their way into our tap water along with environmental heavy metals, chemicals and toxins while standards of testing of these compounds and water quality varies significantly in each municipality across the country. The totality of these environmental chemicals, pollutants and synthetic compounds are unquestionably having an impact on our health.
 The Environmental Pollutant-Neuro-Endocrine-Immune Connection
The Environmental Pollutant-Neuro-Endocrine-Immune Connection
The combination of chronic exposure to immune-triggering pollutants, toxins and inflammatory foods has undoubtedly contributed to various endocrine-related (hormonal) disorders and affected our ability to reproduce healthy offspring. But there is increasing evidence that environmental compounds are contributing to the increase in chronic inflammatory conditions that people suffer from today. Many have theorized that the growing development of autoimmune disease, autism, neurodegenerative disease and other chronic inflammatory conditions may be the result of our recent immunoreactive environment.[8f-10]
Environmental toxins are now being linked with neurodegenerative conditions such as Alzheimer’s and Parkinson’s disease.[11] The unprecedented levels of chemicals and heavy metals today, as well as hybridized, genetically-modified and industrially-processed foods, all activate the immune system toward a pro-inflammatory state.
 Have These Chemicals Been Shown To Be Safe?
Have These Chemicals Been Shown To Be Safe?
Another major problem we face in the U.S. is that only a minority of the synthetic compounds introduced to our environment have been researched individually, much less in conjunction with one another. The Environment Protection Agency (EPA) does not require testing on chemicals introduced to the market unless evidence of potential harm exists, which means testing seldom happens.
“Once substances are suspected of contributing to harm, an administration agency has the burden to show risks or harms and their causes, which is an increasingly difficult demonstration.
In the USA, the vast majority of substances enter commerce without any legally required testing (under the so-called ‘post-market’ laws).
 In 1984, less than 20% of all substances had been subject to pre-market testing and there has been little change since.
In 1984, less than 20% of all substances had been subject to pre-market testing and there has been little change since.
The EPA approves about 90% of new chemicals and only a quarter of more than 80,000 chemicals have been tested for toxicity.”[12]
Lax policies and regulations on commercially available chemicals and toxins in the U.S. have allowed for an environment that has potentially disastrous consequences on human health.
“The legal system and government agencies are not effective in addressing the role of hazardous chemicals and human health”[13]
“Concerns regarding potential risk to the human population from environmental sources are growing at a steady rate”[14]
 Are Our Children Being Exposed?
Are Our Children Being Exposed?
No doubt our children are being exposed to chemicals and toxic compounds at an early age and these are impacting their development before they are even born. Studies are showing startling amounts of environmental chemicals and toxins in the blood supply of embryos during pregnancy!
“Of the 287 chemicals we detected in umbilical cord blood, we know that 180 cause cancer in humans or animals, 217 are toxic to the brain and nervous system and 208 cause birth defects or abnormal development in animal tests”[15]
 More and more evidence is showing our children are not only exposed to these hazardous chemicals in their environment and food supply but are even exposed to extremely high amounts of them through the mother’s breast milk!
More and more evidence is showing our children are not only exposed to these hazardous chemicals in their environment and food supply but are even exposed to extremely high amounts of them through the mother’s breast milk!
“In the first nationwide tests for chemical fire retardants in the breast milk of American women, the Environmental Working Group (EWG) found unexpectedly high levels of these little-known neurotoxic chemicals in every participant tested”
 “The average level of brominated fire retardants in the milk samples was 75 times higher than the average for Swedish women and were at levels associated with toxic effects in several studies using laboratory animals.”[16]
“The average level of brominated fire retardants in the milk samples was 75 times higher than the average for Swedish women and were at levels associated with toxic effects in several studies using laboratory animals.”[16]
Laboratory tests—conducted by one of the world’s leading scientific authorities on fire retardants—found that in 19 of 20 U.S. families, concentrations of toxic fire retardants (PBDEs) were significantly higher in 1.5- to 4-year-old children than their mothers! In total, 11 different flame retardants were found in these children, and 86% of the time the chemicals were present at higher levels in the children than their mothers![17]
In a 2004 paper entitled “A Dialogue on Chemicals and Children”, the World Health Organization made the following statement:
 “It is clear that children may be particularly at risk. Developing organisms, especially during embryonic and fetal periods, early years of life and puberty, go through “windows of susceptibility” during which they are particularly vulnerable to specific environmental stressors. Many of the chemicals known to cause adverse effects easily cross the placenta and can interfere with the growth and development of the fetus. Studies have documented that some solvents and pesticides can cause cancer and that lead, methyl mercury, polychlorinated biphenyls and some pesticides cause neurodevelopmental disorders. We may be conducting a large-scale experiment with children’s health.”[18]
“It is clear that children may be particularly at risk. Developing organisms, especially during embryonic and fetal periods, early years of life and puberty, go through “windows of susceptibility” during which they are particularly vulnerable to specific environmental stressors. Many of the chemicals known to cause adverse effects easily cross the placenta and can interfere with the growth and development of the fetus. Studies have documented that some solvents and pesticides can cause cancer and that lead, methyl mercury, polychlorinated biphenyls and some pesticides cause neurodevelopmental disorders. We may be conducting a large-scale experiment with children’s health.”[18]
Most recently, in September 2013, two prestigious medical organizations – the American Congress of Obstetricians and Gynecologists and the American Society for Reproductive Medicine – said in a joint statement that “toxic chemicals in our environment harm our ability to reproduce, negatively affect pregnancies and are associated with numerous long-term health problems.”
 “Toxic chemicals have long-lasting reproductive health effects…prenatal exposure to certain chemicals is associated with stillbirth, miscarriage, birth defects, childhood cancers and impaired brain development in children.”[19]
“Toxic chemicals have long-lasting reproductive health effects…prenatal exposure to certain chemicals is associated with stillbirth, miscarriage, birth defects, childhood cancers and impaired brain development in children.”[19]
The focus of the remainder of this segment will be examining the top 10 environmental chemicals and toxins taken from the Center for Disease Control and Prevention’s (CDC’s) Agency for Toxic Substances and Disease Registry’s (ATSDR) 2011 Priority List of Hazardous Substances. This represents a list of substances “which are determined to pose the most significant potential threat to human health due to their known or suspected toxicity and potential for human exposure”.[20] We will focus on common exposures of these hazardous compounds and potential impacts on human health. We will also provide simple things you can do immediately to reduce your and your family’s exposure to these hazardous compounds.
Top 10 U.S. Government Priority List of  Hazardous Substances
Hazardous Substances
- Arsenic
- Lead
- Mercury
- Vinyl chloride
- Polychlorinated biphenyls (PCB)
- Benzene
- Cadmium
- Benzopyrene
- Polycyclic aromatic hydrocarbons
- Benzofluoranthene
 1. Arsenic (As)
1. Arsenic (As)
Arsenic is a naturally occurring mineral that is found in high amounts in a variety of foods, particularly rice and poultry, due to human agricultural and farming practices. It is considered #1 in the “Top 10 U.S. Government Priority List of Hazardous Substances”. The U.S. Environmental Protection Agency maximum contaminant level (MCL) in drinking water is 10 µg/L; however, concentrations of over 3,000 µg/L (300 times this limit) have been found in water wells in the United States![21] In 2001, the National Academy of Sciences estimated that people drinking arsenic-contaminated water at 10 parts per billion would have a 1-in-300 risk of developing cancer over their lifetimes. Recent research suggests that people ingest about that much arsenic in a just a half-cup serving of rice, not an unusual amount for millions of Americans![22]
 What are the health effects of arsenic?
What are the health effects of arsenic?
Arsenic is not only a potent human carcinogen (cancer-causing agent) but can also set up children for other health problems later in life. Inorganic arsenic is ranked by the International Agency for Research on Cancer (IARC) as a Group 1 carcinogen. Arsenic is a known carcinogen associated with skin, lung, bladder, kidney, and liver cancer. Dermatological, neurological, respiratory, cardiovascular, immunological, endocrine (hormonal) and childhood developmental effects have also been associated with arsenic exposure. Early-life exposure may be related to increased risks for several types of cancer and other diseases during adulthood.[23]
Studies show exposures of low-to-moderate levels of arsenic (through contaminated tap water, for example) increase risk for the development of pre-malignant skin lesions, high blood pressure, neurological dysfunctions, and all-cause and chronic disease mortality. Arsenic exposure has also been linked to increased risks of internal cancers (described above), diabetes, cardiovascular disease, adverse pregnancy outcomes, and a decrease in children’s intellectual function.[24]
 The good news is the research also indicates that the risk of skin lesion due to arsenic exposure is modifiable by nutritional factors, such as folate and selenium status, lifestyle factors, including cigarette smoking and body mass index, and genetic polymorphisms in genes related to arsenic metabolism. This means you can decrease your risk of skin cancer by supplementing with folic acid and selenium and adopting healthy lifestyle habits such as quitting smoking and maintaining a healthy body weight.[25]
The good news is the research also indicates that the risk of skin lesion due to arsenic exposure is modifiable by nutritional factors, such as folate and selenium status, lifestyle factors, including cigarette smoking and body mass index, and genetic polymorphisms in genes related to arsenic metabolism. This means you can decrease your risk of skin cancer by supplementing with folic acid and selenium and adopting healthy lifestyle habits such as quitting smoking and maintaining a healthy body weight.[25]
Arsenic in baby food?
Many rice-based foods, such as organic rice baby cereal, rice breakfast cereals, brown rice, white rice and some fruit juices have arsenic levels much higher than are allowed in drinking water. Rice absorbs arsenic from soil or water much more effectively than most plants. That’s in part because it is one of the only major crops grown in water-flooded conditions, which allows arsenic to be more easily taken up by its roots and stored in the grains.[26]
 Where does arsenic come from?
Where does arsenic come from?
The U.S. is the world’s leading user of arsenic, and since 1910 about 1.6 million tons have been used for agricultural and industrial purposes. Residues from the decades of use of lead-arsenate insecticides linger in agricultural soil today, even though their use was banned in the 1980s. Other arsenic-containing ingredients in animal feed to prevent disease and promote growth are still permitted. Moreover, fertilizer made from poultry waste can contaminate crops with inorganic arsenic.[27] It turns out that poultry feed is a major ongoing source of arsenic in the environment.
While it might sound alarming that there’s arsenic in your chicken and turkey sandwiches, it’s just one consequence of the use of arsenic in the current poultry industry. Poultry producers often feed their birds antibiotics to combat parasites and enhance the bird’s pink color (for eye appeal to consumers), and one antibiotic commonly used contains arsenic. In addition, poultry waste is widely used as fertilizer, which of course finds its way right into nearby waterways, contaminating them as well as the food grown on those fields.[28]
How to Avoid Exposure: Limit rice consumption and try out alternatives to rice such as quinoa, barley, grits/polenta, couscous or bulgur wheat. Limit poultry consumption and eat organic food whenever possible which may decrease but not eliminate arsenic exposure.
What parents can do to reduce children’s exposure: For babies, try orange vegetables such as sweet potatoes and squash, bananas and avocados as first solid foods. Limit rice consumption. Do not drink rice milk in excess. Eliminate or limit fruit juices to a maximum of one-half cup a day.[29]
 2. Lead (Pb)
2. Lead (Pb)
Lead is a naturally occurring heavy metal found in small amounts in the earth. Industrial activities such as mining, manufacturing, and the burning of fossil fuels are the major sources of environmental lead. Lead was previously used but banned in the U.S. in the manufacture of household paints in 1978 and in gasoline in 1996, which has dramatically reduced exposure. However, environmental exposure to lead in water, soil, and the food supply persists. The major sources of lead in drinking water are lead plumbing, contaminated soil carried into water by rain and wind, and wastewater from industries that use lead.
Where does lead come from?
Lead in soil can be deposited on or absorbed by plants from air pollution. Food can contain lead if these plants are consumed by humans or livestock or during food processing. Lead that gets in or on the plant cannot always be completely removed by washing or other steps in the processing of the food. The major exposure of lead in food is through fruits and grains, according to the Agency for Toxic Substances and Disease Registry. Lead can also get into food through food containers such as older pieces of china and pottery dishes, which are fairly rare.[30]
 What are the health effects of lead?
What are the health effects of lead?
According to a recent review on the effects of lead:
“Lead, a systemic toxicant affecting virtually every organ system, primarily affects the central nervous system, particularly the developing brain. Consequently, children are at a greater risk than adults of suffering from the neurotoxic effects of lead. The ability of lead to pass through the blood-brain barrier is due in large part to its ability to substitute for calcium ions. Within the brain, lead-induced damage in the prefrontal cerebral cortex, hippocampus, and cerebellum can lead to a variety of neurological disorders, such as brain damage, mental retardation, behavioral problems, nerve damage, and possibly Alzheimer’s disease, Parkinson’s disease, and schizophrenia. Experimental studies have also shown that lead exposure may have genotoxic effects, especially in the brain, bone marrow, liver, and lung cells.”[31]
 In children, prenatal and postnatal exposure to lead, even at low levels, is associated with impaired cognitive function and mental development in infants and young children, including reduced IQ and academic achievement [32-36], behavior difficulties such as attention-deficit hyperactive disorder (ADHD)[37,38], and depression and anxiety[39]. Studies have also shown these effects may persist into adulthood.[40,41] Childhood lead exposure has also been associated with decreased brain volume in specific regions of the adult brain responsible for decision-making and mood regulation many years later after exposure.[42]
In children, prenatal and postnatal exposure to lead, even at low levels, is associated with impaired cognitive function and mental development in infants and young children, including reduced IQ and academic achievement [32-36], behavior difficulties such as attention-deficit hyperactive disorder (ADHD)[37,38], and depression and anxiety[39]. Studies have also shown these effects may persist into adulthood.[40,41] Childhood lead exposure has also been associated with decreased brain volume in specific regions of the adult brain responsible for decision-making and mood regulation many years later after exposure.[42]
How to Avoid Exposure: Wash your food before consumption. Avoid lead in paint (pre-1978). If you aren’t sure about the lead in your dishes, you should not use them for storing food.
 3. Mercury (Hg)
3. Mercury (Hg)
Mercury (Hg) is a common contaminant of fish and other seafood. A 1997 analysis of federal health warnings published by the Environmental Working Group (EWG) concluded that fish from more than 1,660 U.S. waterways are so contaminated with mercury that they should not be eaten or eaten only in limited amounts. It found that children and mothers-to-be are at highest risk, not only from fresh fish but from mercury contamination of supermarket products such as canned tuna, shrimp, fish sticks, even instant oatmeal! [43]
On top of this, we may not be getting the most accurate safety information from our governmental agencies’ recommendations. According to a new EWG analysis of fish contaminant and nutrient data published two months ago (January, 2014), people who follow the federal government’s current guidelines on seafood consumption are likely to consume too much mercury or too few beneficial omega-3 fatty acids. [44]
 Why are fish so contaminated with mercury?
Why are fish so contaminated with mercury?
Decades of industrial mercury emissions around the world have contaminated certain fish and seafood, particularly larger, long-lived, deep-water species. A landmark 2009 study by scientists from the U.S. Geological Survey (USGS) has documented how escalating mercury-laden air emissions, chiefly from coal-fired electrical power plants in Asia, are being transformed into methylmercury, which is increasingly polluting the North Pacific Ocean and contaminating tuna, swordfish and other seafood. The study predicts a 50% increase in the Pacific’s mercury level by the year 2050 if mercury emissions from power plants increase according to current projections! [45]
 What are the health effects of mercury exposure?
What are the health effects of mercury exposure?
Many studies show that high exposure to mercury induces changes in the central nervous system (brain), potentially resulting in irritability, fatigue, behavioral changes, tremors, headaches, hearing and cognitive loss, dysarthria (speaking disorder), incoordination, hallucinations, and death. In the cardiovascular system, mercury induces hypertension in humans and animals that has wide-ranging consequences, including alterations in endothelial function. Mercury exposure, even at low doses, affects endothelial and cardiovascular function.[46]
Chronic exposure to mercury vapor can lead to toxic effects to the central nervous system (brain) and the kidneys. Tremor is considered to be the early neurological sign of poisoning by elemental mercury. In addition, damage to peripheral nerves may also occur. Workers exposed to mercury vapor may have abnormalities in sensory and peripheral nerve conduction. Elemental mercury vapor may affect the human immune system and can result in a decreased resistance to infection, cancers, or immune dysregulation that can induce the development of allergy or autoimmune disease.[47]
 Mercury exposure and children’s health
Mercury exposure and children’s health
Acute or chronic mercury (Hg) exposure can cause adverse effects during any period of childhood development. Mercury exposure is especially dangerous to the fetus, newborn infants and young children during critical windows when the brain and other organs are rapidly developing.[48] Studies show that mercury exposure can alter brain development in the fetus, leading to learning problems, reduced performance on intelligence tests and other health problems later in life. According to the CDC, 8% of U.S. women of childbearing age have levels of mercury in their blood that present developmental risks for their babies.[49]
Here are some of the organ systems that have been shown to be impacted in children and infants from prenatal and postnatal mercury exposure.
 Neurological Effects
Neurological Effects
In two large epidemiological studies in New Zealand [50,51] and the Faroe Islands [52-54] associations between prenatal mercury exposure and the neurological development of the children were demonstrated. Outcomes associated with prenatal mercury exposure included the loss of IQ points, and decreased performance of tests, including memory, attention, language, and spatial cognition.[55]
Nephrotoxicity
Inorganic mercury compounds are nephrotoxic (toxic to the kidneys) and can cause kidney damage in children.[56]
Cardiovascular Toxicity
Heart function alteration has been described in children associated with methylmercury exposure from seafood.[57]
 Carcinogenity
Carcinogenity
High exposure to methylmercury is associated with leukemia among adults.[58] Methylmercury compounds are classified as possible carcinogens (cancer-causing agents) to humans (group 2B).
Reproductive Toxicity
One retrospective study examined the effect of methylmercury contamination on the sex ratio of offspring at birth and of fetuses at stillbirth. Due to the severe methylmercury pollution in Minamata, lower numbers of male offspring at birth were found as well as an increase in the quantity of male stillborn fetuses.[59]
Immunotoxicity
Mercury is likely to be immunotoxic, as shown in animal models.[60] The New England children’s Amalgam trial showed an immunotoxic effect in the form of a decline in responsiveness of T cells and monocytes (white blood cells of the immune system).[61]
How to Avoid Exposure: Deep water fish are the most common sources of mercury in food. Limit your consumption of tuna (including canned tuna), swordfish, shrimp and fish sticks. Make sure your fish oil supplements are checked for mercury levels. Visit http://www.ewg.org/ for more information.
 4. Vinyl Chloride (PVC)
4. Vinyl Chloride (PVC)
Vinyl chloride is a colorless organic gas with a sweet odor, and is used to make polyvinyl chloride (PVC) plastic and vinyl products. It is used in the manufacture of numerous products in building and construction, the automotive industry, electrical wire insulation and cables, piping, industrial and household equipment, medical supplies, and is depended upon heavily by the rubber, paper, and glass industries. Over 15 billion pounds were produced in the U.S. in 1995 alone!
 Vinyl chloride is a known human carcinogen
Vinyl chloride is a known human carcinogen
Vinyl chloride is also a known genotoxicant, causing chemical alterations of DNA in tissues that may lead to cancer following exposure of humans and experimental animals. The primary target organ for vinyl chloride exposure is the liver. The association between liver cancer and vinyl chloride exposure is well documented for occupational exposures.[62] Noncancer liver pathologies have also been associated with vinyl chloride exposure.[63] Several studies in experimental animal models have demonstrated that early life exposure to vinyl chloride can increase susceptibility to cancer later in life.[64] Based on these data, the U.S. ATSDR has characterized fetuses, infants, and young children as a “highly susceptible population” for vinyl chloride exposure.
Children are at high risk for exposure to vinyl chloride from air contaminated with vinyl chloride by emissions released from polyvinyl chloride (PVC) plastics production and manufacturing facilities, as well as some incinerators. Contamination of groundwater and drinking water with vinyl chloride-contaminated run-off from such manufacturing facilities is also a concern for exposure of children.[65]
 Vinyl, the most toxic plastic for children’s health
Vinyl, the most toxic plastic for children’s health
Vinyl chloride, also known as vinyl plastic, is considered the most toxic plastic for children’s health and the environment. From production to use and disposal, vinyl releases a toxic cocktail of chemicals including dioxins, phthalates, mercury, PCBs, vinyl chloride, chlorine gas and numerous other substances harmful to our health, some of which are building up in our children’s bodies and food supply. Scientists have found certain vinyl chemicals linked to asthma, cancer, birth defects, learning and developmental disabilities, obesity, diabetes and other preventable chronic diseases. [66]
How to Avoid Exposure: Remove all vinyl from your household, if any, including vinyl flooring or shower curtains, especially if you have children at home. This substance can evaporate into the air at home, unnecessarily exposing you and your family. Drink filtered water to avoid vinyl chloride in drinking water.
 5. Polychlorinated Biphenyls (PCBs)
5. Polychlorinated Biphenyls (PCBs)
Polychlorinated biphenyls (PCBs) are persistent organic pollutants (POPs) that have entered the environment through both use and disposal of these compounds. The environmental transport of PCBs is complex and nearly global in scale. For decades, PCBs were widely used as coolants and insulating fluids (transformer oil) for transformers and capacitors, such as those used in old fluorescent light ballasts, and electric motors. Due to PCBs’ environmental toxicity and classification as a persistent organic pollutant, PCB production was banned by the U.S. Congress in 1979 and by the Stockholm Convention on Persistent Organic Pollutants in 2001. However, despite active research spanning five decades, extensive regulatory actions, and an effective ban on their production since the 1970s, PCBs still persist in the environment and remain a focus of attention. [67]
 Health effects of PCBs
Health effects of PCBs
According to the Environmental Protection Agency (EPA) website:
“PCBs have been demonstrated to cause a variety of adverse health effects. PCBs have been shown to cause cancer in animals. PCBs have also been shown to cause a number of serious non-cancer health effects in animals, including effects on the immune system, reproductive system, nervous system, endocrine system and other health effects. Studies in humans provide supportive evidence for potential carcinogenic and non-carcinogenic effects of PCBs. The different health effects of PCBs may be interrelated, as alterations in one system may have significant implications for the other systems of the body. The body’s regulation of all of these systems is complex and interrelated. As a result, it is not surprising that PCBs can exert a multitude of serious adverse health effects.”[68]
 Endocrine-disrupting effects of persistent organic pollutants
Endocrine-disrupting effects of persistent organic pollutants
Here is an excerpt from one recent 2013 study on the endocrine-disrupting and neurological effects of persistent organic pollutants, such as PCBs:
“Even though high doses of organic pollutants are toxic, relatively low concentrations have been reported to cause long-term alterations in functioning of individual organisms, populations and even next generations. Among these pollutants are dioxins, polychlorinated biphenyls (PCBs), pesticides, brominated flame retardants, plasticizers (bisphenol A and phthalates). In addition to toxic effects, they are able to interfere with hormone receptors, hormone synthesis or hormone conversion. Because these chemicals alter hormone-dependent processes and disrupt functioning of the endocrine glands, they have been classified as endocrine-disrupting chemicals (EDCs). Because certain EDCs are able to alter neural transmission and the formation of neural networks, the term neural-disrupting chemicals has been introduced, thus implicating EDCs in the etiology of neurological disorders. Recently, public concern has been focused on the effects of EDCs on brain function, concomitantly with an increase in neuropsychiatric disorders, including autism, attention deficit and hyperactivity disorder as well as learning disabilities and aggressiveness. Several lines of evidence suggest that exposure to EDCs is associated with depression and could result in neural degeneration.”(69)
 Neurological effects
Neurological effects
Several epidemiological studies provide evidence that PCB exposure during utero alters brain development and the onset of neurological disorders in the developing fetus.[70-73] Multiple studies in human populations have linked exposure to PCBs prior to birth and lower scores on tests of neurological function into infancy and childhood.[74-77] PCB exposure has also been implicated in the development of autism.[78]
In a 2002 Michigan study that tested children at 11 years who were born to women who had eaten relatively large quantities of PCB-contaminated fish, the children most highly exposed to PCBs prior to birth suffered from neurologic deficits which included poorer recognition memory in infancy, lower scores on a preschool IQ test, and poorer verbal IQ and reading comprehension.[79].
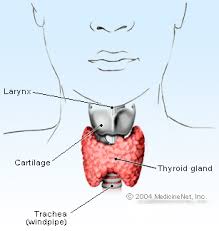 Thyroid and endocrine-disrupting effects
Thyroid and endocrine-disrupting effects
Many studies have shown the endocrine-disrupting effects of PCBs, particularly related to the thyroid.[80-83] A 2012 review of the literature concluded “there is now reasonably firm evidence that PCBs have thyroid-disrupting effects”.[84]
Immunological effects
Several epidemiological studies have shown evidence of immunological impacts of PCB exposure on developing fetuses.[85-88] One recent 2013 systematic review concluded:
“Current epidemiological evidence suggests that early-life exposure to POPs can adversely influence immune and respiratory systems development.”[89]
Cancer
According to the U.S. Environmental Protection Agency:
“Studies in animals provide conclusive evidence that PCBs cause cancer. Studies in humans raise further concerns regarding the potential carcinogenicity of PCBs. Taken together, the data strongly suggest that PCBs are probable human carcinogens.”[90]
Exposure to PCBs
There are two common sources of PCB exposure: farmed salmon and mother’s breast milk.
 Farmed salmon
Farmed salmon
In 2003, the Environmental Working Group (EWG) released results of the most extensive tests to date of polychlorinated biphenyl (PCBs) levels in farmed salmon consumed in the United States. EWG found that the salmon purchased at 7 of 10 local grocery stores was so contaminated with PCBs that they raise cancer-risk concerns, relative to health standards of the U.S. Environmental Protection Agency (EPA).[91]
The EWG analysis of government data also found that farmed salmon are likely the most PCB-contaminated protein source in the current U.S. food supply. Farmed salmon are fattened with ground fishmeal and fish oils that are high in PCBs. As a result, salmon farming operations that produce inexpensive fish unnaturally, concentrate PCBs and have a higher fat content. Farmed salmon contains 52 percent more fat than wild salmon, according to USDA data. EWG analysis of state-of-the-art fish consumption data shows that roughly 800,000 US adults are 100 times over their lifetime allowable cancer risk by eating this contaminated salmon![92]
 Mother’s breast milk
Mother’s breast milk
Mother’s breast milk is known to be a major source of PCBs for infants but PCB exposure from breast milk in infants after birth does not appear to cause significant neurological effects. The risks of neurological effects due to PCB exposure are attributed to fetal exposure to PCBs during fetal development, not after birth. Therefore, breastfeeding is still recommended.
“…nor is there any evidence demonstrating a clinically significant negative effect of postnatal exposure to PCBs via breast milk. To date the majority of studies conclude that despite substantially higher PCB loads among breastfed infants, breastfeeding is still preferable to formula feeding.”[93]
How to Avoid Exposure: Choose wild and canned salmon instead of farmed, and eat an eight-ounce serving of farmed salmon no more than once a month. Make sure your fish oil supplements are checked by the manufacturer for PCB levels. Trim fat from fish before cooking, and choose broiling, baking, or grilling over frying, as these cooking methods allow the PCB-laden fat to cook off the fish.[94]
 6. Benzene
6. Benzene
Benzene is a natural constituent of crude oil, and is one of the most elementary petrochemicals. Benzene is mainly used as a precursor to heavy chemicals, such as ethylbenzene and cumene, which are produced on a billion kilogram scale. Because it has a high octane number, it is an important component of gasoline, comprising a few percent of its mass. Most non-industrial applications have been limited by benzene’s carcinogenicity. Benzene is used mainly as an intermediate to make other chemicals. About 80% of benzene is consumed in the production of three chemicals, ethylbenzene, cumene, and cyclohexane. Its most widely produced derivative is ethylbenzene, precursor to styrene, which is used to make polymers and plastics.[95]
 Vapors from products that contain benzene, such as glues, paints, furniture wax, and detergents, can also be a source of exposure, although many of these have been modified or reformulated since the late 1970s to eliminate or reduce the benzene content. Air around hazardous waste sites or gas stations may contain higher levels of benzene. The petroleum constituents of primary interest to human health have been the aromatic hydrocarbons (i.e.: benzene, ethylbenzene, toluene, and xylenes). Outdoor air may contain low levels of benzene from automobile service stations, wood smoke, tobacco smoke, the transfer of gasoline, exhaust from motor vehicles, and industrial emissions. About 50% of the entire nationwide exposure to benzene results from smoking tobacco or from exposure to tobacco smoke.[96] Benzene is widely used to make other chemicals such as styrofoam, dyes, detergents, drugs, pesticides, and chemicals used in nylon and other synthetic fibers.
Vapors from products that contain benzene, such as glues, paints, furniture wax, and detergents, can also be a source of exposure, although many of these have been modified or reformulated since the late 1970s to eliminate or reduce the benzene content. Air around hazardous waste sites or gas stations may contain higher levels of benzene. The petroleum constituents of primary interest to human health have been the aromatic hydrocarbons (i.e.: benzene, ethylbenzene, toluene, and xylenes). Outdoor air may contain low levels of benzene from automobile service stations, wood smoke, tobacco smoke, the transfer of gasoline, exhaust from motor vehicles, and industrial emissions. About 50% of the entire nationwide exposure to benzene results from smoking tobacco or from exposure to tobacco smoke.[96] Benzene is widely used to make other chemicals such as styrofoam, dyes, detergents, drugs, pesticides, and chemicals used in nylon and other synthetic fibers.
 In 2006, the Food and Drug Administration (FDA) announced it found high levels of benzene in several samples in a test of a small number of sodas and juice drinks. In a very limited sample of products, FDA found two popular drinks—Safeway Diet Orange and Crystal Light Sunrise Classic Orange—with up to 17 times more benzene than allowed in tap water, and three other products with benzene levels up to four times the drinking water limit. Many other products had detectable levels of the carcinogen.[97] This is particularly disturbing given that in 1990, the FDA learned that certain soft drinks marketed to children contain two ingredients, ascorbic acid (vitamin C) and either sodium benzoate or potassium benzoate, that can mix in the soda to form benzene.[98]
In 2006, the Food and Drug Administration (FDA) announced it found high levels of benzene in several samples in a test of a small number of sodas and juice drinks. In a very limited sample of products, FDA found two popular drinks—Safeway Diet Orange and Crystal Light Sunrise Classic Orange—with up to 17 times more benzene than allowed in tap water, and three other products with benzene levels up to four times the drinking water limit. Many other products had detectable levels of the carcinogen.[97] This is particularly disturbing given that in 1990, the FDA learned that certain soft drinks marketed to children contain two ingredients, ascorbic acid (vitamin C) and either sodium benzoate or potassium benzoate, that can mix in the soda to form benzene.[98]
 Health effects of benzene
Health effects of benzene
Acute (short-term) inhalation exposure of humans to benzene may cause drowsiness, dizziness, headaches, as well as eye, skin, and respiratory tract irritation, and, at high levels, unconsciousness. Chronic (long-term) inhalation exposure has caused various disorders in the blood, including reduced numbers of red blood cells and aplastic anemia. Reproductive effects have been reported for women exposed by inhalation to high levels, and adverse effects on the developing fetus have been observed in animal tests. Increased incidence of leukemia (cancer of the tissues that form white blood cells) have been observed in humans occupationally exposed to benzene. Benzene has been classified by the EPA as a known human carcinogen for all routes of exposure. [99]
How to Avoid Exposure: Avoid tobacco and inhalation of all smoke. Avoid inhalation of gasoline exhaust or emissions. Avoid unnecessary air pollution. Buy simple and natural cleaning products when possible. Eat organic whenever possible.
 7. Cadmium
7. Cadmium
Human exposures to environmental cadmium are primarily the result of fossil fuel combustion, phosphate fertilizers, natural sources, iron and steel production, cement production and related activities, nonferrous metals production, and municipal solid waste incineration. The use of cadmium is generally decreasing due to its toxicity and the replacement of nickel-cadmium batteries with nickel-metal hydride and lithium-ion batteries.[100]
 Tobacco smoking is the most important single source of cadmium exposure in the general population. On average, smokers have 4–5 times higher blood cadmium concentrations and 2–3 times higher kidney cadmium concentrations than non-smokers. Despite the high cadmium content in cigarette smoke, there seems to be little exposure to cadmium from passive smoking.[101]
Tobacco smoking is the most important single source of cadmium exposure in the general population. On average, smokers have 4–5 times higher blood cadmium concentrations and 2–3 times higher kidney cadmium concentrations than non-smokers. Despite the high cadmium content in cigarette smoke, there seems to be little exposure to cadmium from passive smoking.[101]
Many foods contain cadmium and contribute to the cadmium in modern populations including leafy vegetables, grains, breads, legumes, and kidney meat. Other foods that are rich in cadmium which can greatly increase the cadmium concentration in human bodies are liver, mushrooms, shellfish, mussels, cocoa powder and dried seaweed.[102]
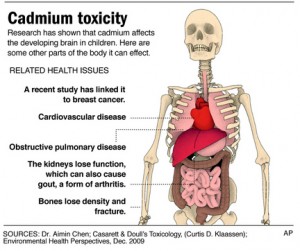 Health effects of cadmium
Health effects of cadmium
Cadmium exposure is a risk factor associated with early atherosclerosis and hypertension, which can both lead to cardiovascular disease.[103] According to the Center for Disease Control and Prevention’s (CDC) Agency for Toxic Substances and Disease Registry (ATSDR), cadmium is a known human carcinogen and affects the following organ systems: cardiovascular (heart and blood vessels), developmental (effects during periods when organs are developing), gastrointestinal (digestive), neurological (nervous system), renal (urinary system or kidneys), reproductive (producing children), respiratory (from the nose to the lungs).[104,105]
How to Avoid Exposure: Avoid tobacco and inhalation of all smoke. Be aware of cadmium-rich foods and over-consuming contaminated sources of these.
 8., 9., 10. Benzopyrene, Benzofluoranthene and Polycyclic Aromatic Hydrocarbons (PAHs)
8., 9., 10. Benzopyrene, Benzofluoranthene and Polycyclic Aromatic Hydrocarbons (PAHs)
Polycyclic aromatic hydrocarbons (PAHs) occur in oil, coal, and tar deposits, and are produced as byproducts of fuel burning (whether fossil fuel or biomass). They are potent atmospheric pollutants. PAHs are one of the most widespread organic pollutants. In addition to their presence in fossil fuels they are also formed by incomplete combustion of carbon-containing fuels such as wood, coal, diesel, fat, tobacco, and incense. Different types of combustion yield different distributions of PAHs in both relative amounts of individual PAHs and in which isomers are produced. PAH chemicals are often linked to oil spills. Following the massive Deepwater Horizon oil spill, scientists found PAH levels to be 40 times higher than before the area was affected. The researchers said that the compounds can enter the food chain through organisms such as plankton or fish. One PAH compound, benzopyrene, is notable for being the first chemical carcinogen to be discovered (and is one of many carcinogens found in cigarette smoke). The EPA has classified seven different PAH compounds as probable human carcinogens, including benzofluoranthene.[106]
 Health effects of polycyclic aromatic hydrocarbons (PAHs)
Health effects of polycyclic aromatic hydrocarbons (PAHs)
High prenatal exposure to PAHs is associated with lower IQ and childhood asthma.[107] The Center for Children’s Environmental Health reports studies that demonstrate that exposure to PAH pollution during pregnancy is related to adverse birth outcomes including low birth weight, premature delivery, and heart malformations. Cord blood of exposed babies shows DNA damage that has been linked to cancer.[108]
In a 2009 study, researchers from the University of Cincinnati and Columbia University, NY reported that traffic pollution causes genetic changes in the womb that increase a child’s risk of developing asthma. The culprit is prenatal exposure to polycyclic aromatic hydrocarbons (PAHs), which are created as byproducts of incomplete combustion of carbon-containing fuels such as gasoline. PAH levels are high in the air in heavy-traffic areas, posing health risk for inner-city neighborhoods and residential communities in proximity to major highways.[109]
 In addition, a 2012 Columbia University study in Environmental Health Perspectives linked prenatal exposure to these pollutants and eventual child behavioral outcomes. The study found that exposure to higher levels of PAHs was associated with a 24% higher score of anxiety/depression for children ages 6 to 7 than those with low exposure levels. Infants found to have elevated PAH levels in their umbilical cord blood were 46% more likely to eventually score highly on the anxiety/depression scale than those with low PAH levels in cord blood.[110]
In addition, a 2012 Columbia University study in Environmental Health Perspectives linked prenatal exposure to these pollutants and eventual child behavioral outcomes. The study found that exposure to higher levels of PAHs was associated with a 24% higher score of anxiety/depression for children ages 6 to 7 than those with low exposure levels. Infants found to have elevated PAH levels in their umbilical cord blood were 46% more likely to eventually score highly on the anxiety/depression scale than those with low PAH levels in cord blood.[110]
How to Avoid Exposure: Avoid tobacco and all smoke. Avoid inhalation of gasoline exhaust or emissions. Avoid unnecessary air pollution.
References
1. Moreno MA, Furtner F, Rivara FP. Children’s environmental health. Arch Pediatr Adolesc Med. 2012 Oct;166(10):976. doi: 10.1001/2013.jamapediatrics.8.
2. Amy M. Branum, Susan L. Lukacs. Food Allergy Among U.S. Children: Trends in Prevalence and Hospitalizations. NCHS Data Brief. No.10. October 2008
3. Gupta RS1, Springston EE, Warrier MR, Smith B, Kumar R, Pongracic J, Holl JL. The prevalence, severity, and distribution of childhood food allergy in the United States. Pediatrics. 2011 Jul;128(1):e9-17. doi: 10.1542/peds.2011-0204. Epub 2011 Jun 20.
4. Gupta RS1, Springston EE, Warrier MR, Smith B, Kumar R, Pongracic J, Holl JL. The prevalence, severity, and distribution of childhood food allergy in the United States. Pediatrics. 2011 Jul;128(1):e9-17. doi: 10.1542/peds.2011-0204. Epub 2011 Jun 20.
5. Gupta RS1, Springston EE, Warrier MR, Smith B, Kumar R, Pongracic J, Holl JL. The prevalence, severity, and distribution of childhood food allergy in the United States. Pediatrics. 2011 Jul;128(1):e9-17. doi: 10.1542/peds.2011-0204. Epub 2011 Jun 20.
6. Amy M. Branum, Susan L. Lukacs. Food Allergy Among U.S. Children: Trends in Prevalence and Hospitalizations. NCHS Data Brief. No.10. October 2008
7. Amy M. Branum, Susan L. Lukacs. Food Allergy Among U.S. Children: Trends in Prevalence and Hospitalizations. NCHS Data Brief. No.10. October 2008
8a. http://www.theguardian.com/commentisfree/cifamerica/2011/jun/10/prescription-drug-abuse
8b. http://www.cdc.gov/nchs/data/databriefs/db42.htm
8c. http://www.cdc.gov/nchs/data/databriefs/db42.htm
8d. http://apps.who.int/medicinedocs/en/d/Js6160e/6.html
8e. http://apps.who.int/medicinedocs/documents/s19032en/s19032en.pdf
8f. Volk HE, Lurmann, F, Penfold B, Hertz-Picciotto I, McConnell R. Traffic-related air pollution, particulate matter and autism. JAMA Psychiatry. 2013 Jan;70(1):71-7
9. Calderon-Garcidenuas L, Mora-Tiscareno A, et al. White matter hyperintensities, systemic inflammation, brain growth and cognitive functions in children exposed to air pollution. J Alzheimer’s Dis. 2012;31(1):183-191
10. Powell JJ, Van de Water, Gershwin ME. Evidence for the role of environmental agents in the initiation or progression of autoimmune conditions. Environ Health Perspect. 1999 Oct;107 Suppl 5:667-72
11. Stein J, Schettler T, Rohrer B, Valenti M. Environmental threats to healthy aging. Greater Boston Phys for Soc. Respons.and Science and Environ. Health Network. July, 2008. http://www.agehealthy.org/pdf/GBPSRSEHN_HealthyAging1017.pdf
12. Cranor C. The legal failure to prevent subclinical developmental toxicity. Basic Clin Pharmacol Toxicol. 2008 Feb;102(2):267-73
13. Cranor C. The legal failure to prevent subclinical developmental toxicity. Basic Clin Pharmacol Toxicol. 2008 Feb;102(2):267-73
14. Jan AT, Ali A, Haq Q. Glutathione as an antioxidant in inorganic mercury induced nephrotoxicity. J Postgrad Med. 2011 Jan-Mar;57(1):72-77
15. Houlihan J, et al. Body burden: the pollution in newborns. July 14, 2005. Environmental Working Group. http//www.ewg.org/research/body-burden-pollution-newborns
16. Lunder S, Sharp R. Toxic fire retardants in human breast milk. Sept 23, 2003. Environmental Working Group. http//www.ewg.org/research/mothers-milk-0
17. http://www.ewg.org/research/fire-retardants-toddlers-and-their-mothers
18. http://www.who.int/bulletin/volumes/82/11/editorial31104html/en/
20. http://www.atsdr.cdc.gov/SPL/index.html
21. Marisa F. Naujokas, Beth Anderson, Habibul Ahsan, H. Vasken Aposhian, Joseph H. Graziano, Claudia Thompson, William A. Suk. The Broad Scope of Health Effects from Chronic Arsenic Exposure: Update on a Worldwide Public Health Problem. Environ Health Perspect. 2013 March; 121(3): 295–302. Published online 2013 January 3. doi: 10.1289/ehp.1205875
22. http://www.ewg.org/enviroblog/2012/09/getting-arsenic-out-your-and-your-kids-diet
23. Marisa F. Naujokas, Beth Anderson, Habibul Ahsan, H. Vasken Aposhian, Joseph H. Graziano, Claudia Thompson, William A. Suk. The Broad Scope of Health Effects from Chronic Arsenic Exposure: Update on a Worldwide Public Health Problem. Environ Health Perspect. 2013 March; 121(3): 295–302. Published online 2013 January 3. doi: 10.1289/ehp.1205875
24. Yu Chen, Faruque Parvez, Mary Gamble, Tariqul Islam, Alauddin Ahmed, Maria Argos, Joseph H. Graziano, Habibul Ahsan. Arsenic Exposure at Low-to-Moderate Levels and Skin Lesions, Arsenic Metabolism, Neurological Functions, and Biomarkers for Respiratory and Cardiovascular Diseases: Review of Recent Findings from the Health Effects of Arsenic Longitudinal Study (HEALS) in Bangladesh. Toxicol Appl Pharmacol. Author manuscript; available in PMC 2014 January 28.
Published in final edited form as: Toxicol Appl Pharmacol. 2009 September 1; 239(2): 184–192. Published online 2009 January 27.
25. Yu Chen, Faruque Parvez, Mary Gamble, Tariqul Islam, Alauddin Ahmed, Maria Argos, Joseph H. Graziano, Habibul Ahsan. Arsenic Exposure at Low-to-Moderate Levels and Skin Lesions, Arsenic Metabolism, Neurological Functions, and Biomarkers for Respiratory and Cardiovascular Diseases: Review of Recent Findings from the Health Effects of Arsenic Longitudinal Study (HEALS) in Bangladesh. Toxicol Appl Pharmacol. Author manuscript; available in PMC 2014 January 28.
Published in final edited form as: Toxicol Appl Pharmacol. 2009 September 1; 239(2): 184–192. Published online 2009 January 27.
26. http://www.ewg.org/enviroblog/2012/09/getting-arsenic-out-your-and-your-kids-diet
27. http://www.consumerreports.org/cro/magazine/2012/11/arsenic-in-your-food/index.htm
28. http://www.ewg.org/enviroblog/2010/11/turkeys-arsenic-arsenic-out
29. http://www.ewg.org/release/reducing-arsenic-your-diet
30. http://extoxnet.orst.edu/faqs/foodcon/lead.htm
31. Talia Sanders, Yiming Liu, Virginia Buchner, Paul B. Tchounwou. Neurotoxic Effects and Biomarkers of Lead Exposure: A Review. Rev Environ Health. Author manuscript; available in PMC 2010 April 22.
Published in final edited form as: Rev Environ Health. 2009 Jan–Mar; 24(1): 15–45.
32. Wieslaw Jedrychowski, Frederica P. Perera, Jeffery Jankowski, Dorota Mrozek-Budzyn, Elzbieta Mroz, Elzbieta Flak, Susan Edwards, Anita Skarupa, Ilona Lisowska-Miszczyk. Very Low Prenatal Exposure to Lead and Mental Development of Children in Infancy and Early Childhood: Krakow Prospective Cohort Study. Neuroepidemiology. 2009 April; 32(4): 270–278. Published online 2009 February 18. doi: 10.1159/000203075
33. Meeyoung O. Min, Lynn T. Singer, H. Lester Kirchner, Sonia Minnes, Elizabeth Short, Zehra Hussain, Suchitra Nelson. Cognitive Development and Low-Level Lead Exposure in Poly-Drug Exposed Children
Neurotoxicol Teratol. Author manuscript; available in PMC 2010 July 1. Published in final edited form as: Neurotoxicol Teratol. 2009; 31(4): 225–231. Published online 2009 April 2. doi: 10.1016/j.ntt.2009.03.002
34. Roberto G Lucchini, Silvia Zoni, Stefano Guazzetti, Elza Bontempi, Serena Micheletti, Karin Broberg, Giovanni Parrinello, Donald R Smith. Inverse association of intellectual function with very low blood lead but not with manganese exposure in Italian adolescents. Environ Res. Author manuscript; available in PMC 2013 October 1. Published in final edited form as: Environ Res. 2012 October; 118: 65–71. Published online 2012 August 24. doi: 10.1016/j.envres.2012.08.003
35. Canfield RL, et al. Intellectual impairment in children with blood lead concentrations below 10 microg per deciliter. N Engl J Med. 2003;348:1517–26.
36. Lanphear BP, et al. Low-level environmental lead exposure and children’s intellectual function: an international pooled analysis. Environ Health Perspect. 2005;113:894–9.
37. Paul A. Eubig, Andréa Aguiar, Susan L. Schantz. Lead and PCBs as Risk Factors for Attention Deficit/Hyperactivity Disorder. Environ Health Perspect. 2010 December; 118(12): 1654–1667. Published online 2010 September 9. doi: 10.1289/ehp.0901852.
38. Nigg JT, et al. Low blood lead levels associated with clinically diagnosed attention-deficit/hyperactivity disorder and mediated by weak cognitive control. Biol Psychiatry. 2008;63:325–31.
39. Ki-Do Eum, Susan A. Korrick, Jennifer Weuve, Olivia Okereke, Laura D. Kubzansky, Howard Hu, Marc G. Weisskopf. Relation of Cumulative Low-Level Lead Exposure to Depressive and Phobic Anxiety Symptom Scores in Middle-Age and Elderly Women. Environ Health Perspect. 2012 June; 120(6): 817–823. Published online 2012 February 29. doi: 10.1289/ehp.1104395
40. Mazumdar M, et al. Prenatal Lead Levels, Plasma Amyloid beta Levels and Gene Expression in Young Adulthood. Environ Health Perspect 2012
41. Needleman HL, et al. The long-term effects of exposure to low doses of lead in childhood. An 11-year follow-up report. N Engl J Med. 1990;322:83–8.
42. Kim M Cecil, Christopher J Brubaker, Caleb M Adler, Kim N Dietrich, Mekibib Altaye, John C Egelhoff, Stephanie Wessel, Ilayaraja Elangovan, Richard Hornung, Kelly Jarvis, Bruce P Lanphear. Decreased Brain Volume in Adults with Childhood Lead Exposure. PLoS Med. 2008 May; 5(5): e112. Published online 2008 May 27. doi: 10.1371/journal.pmed.0050112
43. http://www.ewg.org/research/catching-limit/news-release-epa-16-million-kids-moms-risk
45. http://www.ewg.org/news/news-releases/2009/05/06/mercury-fish-predicted-soar
46. Bruna Fernandes Azevedo, Lorena Barros Furieri, Franck Maciel Peçanha, Giulia Alessandra Wiggers, Paula Frizera Vassallo, Maylla Ronacher Simões, Jonaina Fiorim, Priscila Rossi de Batista, Mirian Fioresi, Luciana Rossoni, Ivanita Stefanon, María Jesus Alonso, Mercedes Salaices, Dalton Valentim Vassallo. Toxic Effects of Mercury on the Cardiovascular and Central Nervous Systems. J Biomed Biotechnol. 2012; 2012: 949048. Published online 2012 July 2. doi: 10.1155/2012/949048
47. Jung-Duck Park, Wei Zheng. Human Exposure and Health Effects of Inorganic and Elemental Mercury. J Prev Med Public Health. 2012 November; 45(6): 344–352. Published online 2012 November 29. doi: 10.3961/jpmph.2012.45.6.344
48. Stephan Bose-O’Reilly, Kathleen M. McCarty, Nadine Steckling, Beate Lettmeier. Mercury Exposure and Children’s Health. Curr Probl Pediatr Adolesc Health Care. Author manuscript; available in PMC 2011 May 17. Published in final edited form as: Curr Probl Pediatr Adolesc Health Care. 2010 September; 40(8): 186–215. doi: 10.1016/j.cppeds.2010.07.002
50. Kjellstrom T, Kennedy P, Wallis S, Mantell C. Physical and Mental Development of Children with Prenatal Exposure to Mercury from Fish. Stage I: Preliminary Tests at Age 4. National Swedish Environmental Protection Board; Solna, Sweden: 1986.
51. Kjellstrom T, Kennedy P, Wallis S, Stewart A, Friberg L, Lind B. Physical and Mental Development of Children with Prenatal Exposure to Mercury from Fish. Stage II: Interviews and Psychological Tests at Age 4. National Swedish Environmental Protection Board; Solna, Sweden: 1989.
52. Grandjean P, Weihe P, Jorgensen PJ, Clarkson T, Cernichiari E, Videro T. Impact of maternal seafood diet on fetal exposure to mercury, selenium, and lead. Arch Environ Health. 1992;47:185–95.
53. Grandjean P, Weihe P, White RF. Milestone development in infants exposed to methylmercury from human milk. Neurotoxicology. 1995;16:27–33.
54. Grandjean P, Weihe P, White RF, Debes F, Araki S, Yokoyama K, et al. Cognitive deficit in 7-year-old children with prenatal exposure to methylmercury. Neurotoxicol Teratol. 1997;19:417–28.
55. Stephan Bose-O’Reilly, Kathleen M. McCarty, Nadine Steckling, Beate Lettmeier. Mercury Exposure and Children’s Health. Curr Probl Pediatr Adolesc Health Care. Author manuscript; available in PMC 2011 May 17. Published in final edited form as: Curr Probl Pediatr Adolesc Health Care. 2010 September; 40(8): 186–215. doi: 10.1016/j.cppeds.2010.07.002
56. Stephan Bose-O’Reilly, Kathleen M. McCarty, Nadine Steckling, Beate Lettmeier. Mercury Exposure and Children’s Health. Curr Probl Pediatr Adolesc Health Care. Author manuscript; available in PMC 2011 May 17. Published in final edited form as: Curr Probl Pediatr Adolesc Health Care. 2010 September; 40(8): 186–215. doi: 10.1016/j.cppeds.2010.07.002
57. Grandjean P, Murata K, Budtz-Jorgensen E, Weihe P. Cardiac autonomic activity in methylmercury neurotoxicity: 14-year follow-up of a Faroese birth cohort. J Pediatr. 2004;144:169–76.
58. Yorifuji T, Tsuda T, Kawakami N. Age standardized cancer mortality ratios in areas heavily exposed to methyl mercury. Int Arch Occup Environ Health. 2007;80:679–88.
59. Sakamoto M, Nakano A, Akagi H. Declining Minamata male birth ratio associated with increased male fetal death due to heavy methylmercury pollution. Environ Res. 2001;87:92–8.
60. World Health Organization Principles and methods for assessing autoimmunity associated with exposure to chemicals. Environmental Health Criteria. 2006;236:1–333.
61. Shenker BJ, Maserejian NN, Zhang A, McKinlay S. Immune function effects of dental amalgam in children: a randomized clinical trial. J Am Dent Assoc. 2008;139:1496–505.
62. Sherman M. Vinyl chloride and the liver. J Hepatol. 2009 Dec;51(6):1074-81. doi: 10.1016/j.jhep.2009.09.012. Epub 2009 Oct 1.
63. Sherman M. Vinyl chloride and the liver. J Hepatol. 2009 Dec;51(6):1074-81. doi: 10.1016/j.jhep.2009.09.012. Epub 2009 Oct 1.
64. http://www.epa.gov/teach/chem_summ/VC_summary.pdf
65. http://www.epa.gov/teach/chem_summ/VC_summary.pdf
66. http://chej.org/backtoschool2013/
67. http://en.wikipedia.org/wiki/Polychlorinated_biphenyls#United_States
68. http://www.epa.gov/epawaste/hazard/tsd/pcbs/pubs/effects.htm
69. Kajta M, Wójtowicz AK. Impact of endocrine-disrupting chemicals on neural development and the onset of neurological disorders. Pharmacol Rep. 2013;65(6):1632-9.
70. Crinnion WJ. Polychlorinated biphenyls: persistent pollutants with immunological, neurological, and endocrinological consequences. Altern Med Rev. 2011 Mar;16(1):5-13. Review.
71. Faroon O, Jones D, de Rosa C. Effects of polychlorinated biphenyls on the nervous system.
Toxicol Ind Health. 2000 Sep;16(7-8):305-33. Review.
72. Jones DC, Miller GW. The effects of environmental neurotoxicants on the dopaminergic system: A possible role in drug addiction. Biochem Pharmacol. 2008 Sep 1;76(5):569-81. doi: 10.1016/j.bcp.2008.05.010. Epub 2008 May 20. Review.
73. Carpenter DO. Polychlorinated biphenyls (PCBs): routes of exposure and effects on human health. Rev Environ Health. 2006;21:1–23.
74. Schantz SL, Widholm JJ, Rice DC. Effects of PCB exposure on neuropsychological function in children. Environ Health Perspect. 2003;111:357–576.
75. Stewart P, Reihman J, Gump B, Lonky E, Darvill T, Pagano J. Response inhibition at 8 and 9 1/2 years of age in children prenatally exposed to PCBs. Neurotoxicol Teratol. 2005;27:771–80.
76. Jacobson JL, Jacobson SW. Prenatal exposure to polychlorinated biphenyls and attention at school age. J Pediatr. 2003;143:780–788.
77. Ribas-Fitó N, Sala M, Kogevinas M, Sunyer J. Polychlorinated biphenyls (PCBs) and neurological development in children: a systematic review. J Epidemiol Community Health. 2001 Aug;55(8):537-46. Review.
78. Pessah IN, Seegal RF, Lein PJ, LaSalle J, Yee BK, Van De Water J, Berman RF. Immunologic and neurodevelopmental susceptibilities of autism. Neurotoxicology. 2008 May;29(3):532-45. doi: 10.1016/j.neuro.2008.02.006. Epub 2008 Feb 23. Review.
79. Jacobson JL, Jacobson SW. Association of prenatal exposure to an environmental contaminant with intellectual function in childhood. J Toxicol Clin Toxicol. 2002;40(4):467-75.
80. Crinnion WJ. Polychlorinated biphenyls: persistent pollutants with immunological, neurological, and endocrinological consequences. Altern Med Rev. 2011 Mar;16(1):5-13. Review.
81. Jugan ML, Levi Y, Blondeau JP. Endocrine disruptors and thyroid hormone physiology.
Biochem Pharmacol. 2010 Apr 1;79(7):939-47. doi: 10.1016/j.bcp.2009.11.006. Epub 2009 Nov 12. Review.
82. Boas M, Main KM, Feldt-Rasmussen U. Environmental chemicals and thyroid function: an update.
Curr Opin Endocrinol Diabetes Obes. 2009 Oct;16(5):385-91. doi: 10.1097/MED.0b013e3283305af7. Review.
83. Massart F, Meucci V. Environmental thyroid toxicants and child endocrine health. Pediatr Endocrinol Rev. 2007 Sep;5(1):500-9.
84. Boas M, Feldt-Rasmussen U, Main KM. Thyroid effects of endocrine disrupting chemicals. Mol Cell Endocrinol. 2012 May 22;355(2):240-8. doi: 10.1016/j.mce.2011.09.005. Epub 2011 Sep 10. Review.
85. Crinnion WJ. Polychlorinated biphenyls: persistent pollutants with immunological, neurological, and endocrinological consequences. Altern Med Rev. 2011 Mar;16(1):5-13. Review.
86. White SS, Birnbaum LS. An overview of the effects of dioxins and dioxin-like compounds on vertebrates, as documented in human and ecological epidemiology. J Environ Sci Health C Environ Carcinog Ecotoxicol Rev. 2009 Oct;27(4):197-211. doi: 10.1080/10590500903310047. Review.
87. Pessah IN, Seegal RF, Lein PJ, LaSalle J, Yee BK, Van De Water J, Berman RF. Immunologic and neurodevelopmental susceptibilities of autism. Neurotoxicology. 2008 May;29(3):532-45. doi: 10.1016/j.neuro.2008.02.006. Epub 2008 Feb 23. Review.
88. Nagayama J, Tsuji H, Iida T, Nakagawa R, Matsueda T, Hirakawa H, Yanagawa T, Fukushige J, Watanabe T. Immunologic effects of perinatal exposure to dioxins, PCBs and organochlorine pesticides in Japanese infants. Chemosphere. 2007 Apr;67(9):S393-8. Epub 2007 Jan 11.
89. Gascon M, Morales E, Sunyer J, Vrijheid M. Effects of persistent organic pollutants on the developing respiratory and immune systems: a systematic review. Environ Int. 2013 Feb;52:51-65. doi: 10.1016/j.envint.2012.11.005. Epub 2013 Jan 3. Review.
90. http://www.epa.gov/wastes/hazard/tsd/pcbs/pubs/effects.htm
93. Jorissen J. Literature review. Outcomes associated with postnatal exposure to polychlorinated biphenyls (PCBs) via breast milk. Adv Neonatal Care. 2007 Oct;7(5):230-7. Review.
94. http://www.ewg.org/research/pcbs-farmed-salmon/recommendations
95. http://en.wikipedia.org/wiki/Benzene
96. http://www.ewg.org/research/stolen-inventory/chemicals-concern
97. http://www.ewg.org/news/news-releases/2006/05/19/fda-finds-high-benzene-levels-limited-test-drinks
99. http://www.epa.gov/ttn/atw/hlthef/benzene.html
100. http://en.wikipedia.org/wiki/Cadmium
101. Jarup, L. Health effects of cadmium exposure—a review of the literature and a risk estimate. Scandinavian Journal of Work, Environment and Health. 1998. 24: 11–51.
102. http://www.lenntech.com/periodic/elements/cd.htm
103. Cadmium Exposure can Induce Early Atherosclerotic Changes, Medinews Direct, 7 September 2009
104. http://www.atsdr.cdc.gov/substances/toxsubstance.asp?toxid=15
105. Soisungwan Satarug, Scott H. Garrett, Mary Ann Sens, Donald A. Sens. Cadmium, Environmental Exposure, and Health Outcomes. Environ Health Perspect. 2010 February; 118(2): 182–190. Published online 2009 October 5. doi: 10.1289/ehp.0901234
106. http://en.wikipedia.org/wiki/Polycyclic_aromatic_hydrocarbon
108. http://www.ccceh.org/pdf-press/Time10-4-10.pdf
109. http://www.plosone.org/article/info%3Adoi%2F10.1371%2Fjournal.pone.0004488
110. Perera, Frederica P.; Tang, Deliang; Wang, Shuang; Vishnevetsky, Julia (2012). Prenatal Polycyclic Aromatic Hydrocarbon (PAH) Exposure and Child Behavior at age 6-7. Environmental Health Perspectives. doi:10.1289/ehp.1104315
