Introductory Note
There is currently a wealth of information on the coronavirus that causes COVID-19 including how this virus impacts health as well as recommendations for various interventions to protect oneself from this illness. However, in many cases, the scientific basis of these recommendations are questionable. The purpose of the following article is to review some of the scientific literature on this topic and provide an evidence-based rationale for the prevention and immune resistance of viral challenges, such as the one resulting from the coronavirus responsible for the current pandemic.
Immune Resistance to COVID-19
The coronavirus that causes the disease known as COVID-19 is called SARS-COV2 and is closely related to the viruses that caused SARS (Sudden Acute Respiratory Syndrome) in the 2002 outbreak and MERS (Middle Eastern Respiratory Syndrome) in the 2012 and 2015 outbreaks. All of these diseases were caused by infections of the respiratory tract by the coronavirus. Before 2019, there were six coronaviruses that could infect humans and cause respiratory disease but most of these only affected the upper respiratory tract and caused symptoms similar to the common cold. The new SARS-COV2, like the viruses that caused SARS and MERS, can infect the lower respiratory tract and cause severe pneumonia, inflammation and respiratory distress in humans in a very short period of time. However, unlike the other viruses, it is able to spread even when people have mild to no symptoms.
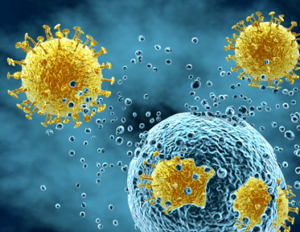
Viral Replication

Viruses are classified as either ‘enveloped’ or ‘naked’, depending on whether the protein shell (called a ‘capsid’) is surrounded by an outer membrane. Coronaviruses are enveloped, positive-stranded RNA viruses which replicate by binding to human cell receptors, entering the cells and high-jacking the cell’s genetic machinery to reproduce viral components. New viruses are assembled from these components which eventually burst out of the cells causing cell destruction and are then able to infect other cells and begin replication all over again.
Transmission
Like influenza and viral pneumonia, these SARS-COV2 primarily affect the lungs and is spread primarily through respiratory droplets and direct contact with body secretions. The infection stimulates coughing and sneezing which enables the virus to spread. Many people who are infected have mild to no symptoms but act as carriers or vectors, spreading the virus throughout the population unknowingly. It seems also that the virus can survive for as long as 48 hours on some surfaces, thus being transmitted in some cases by contact with those surfaces followed by hand-to-mouth contact.
Infectiousness
 The infectiousness of the SARS-COV2 virus is the major factor in its ability to spread because many people are contagious with mild to no symptoms. This is an important difference between the original SARS and MERS virus outbreaks. Although those viruses were more deadly, people generally displayed signs of sickness when they were contagious so the virus did not spread as easily. The original SARS had a mortality rate of around 16%. Although not yet known, current estimates of the mortality rate of SARS-COV2 is about 1.0-2.0% so the original SARS was probably about 10 to 16 times higher than the current outbreak. MERS was around 30%, so that’s 20 to 30 times higher than SARS-COV2. In comparison, the influenza virus that causes the flu has a mortality rate of 0.1 to 0.2%, making SARS-COV2 about 10 times as deadly as the flu.
The infectiousness of the SARS-COV2 virus is the major factor in its ability to spread because many people are contagious with mild to no symptoms. This is an important difference between the original SARS and MERS virus outbreaks. Although those viruses were more deadly, people generally displayed signs of sickness when they were contagious so the virus did not spread as easily. The original SARS had a mortality rate of around 16%. Although not yet known, current estimates of the mortality rate of SARS-COV2 is about 1.0-2.0% so the original SARS was probably about 10 to 16 times higher than the current outbreak. MERS was around 30%, so that’s 20 to 30 times higher than SARS-COV2. In comparison, the influenza virus that causes the flu has a mortality rate of 0.1 to 0.2%, making SARS-COV2 about 10 times as deadly as the flu.
Clinical Presentation
Common symptoms of COVID-19 include fever, fatigue, and dry cough. A few patients have symptoms such as nasal congestion, runny nose, sore throat, and diarrhea. Some patients only have a low fever and mild fatigue. In severe cases, the infection can cause pneumonia, shortness of breath and breathing difficulties. Critical patients may progress rapidly to acute respiratory distress syndrome (ARDS), septic shock and even death.
Pathogenesis
As with SARS, COVID-19 disease occurs in stages: first, there is initial infection that allows viral replication, spread of the viral infection throughout the respiratory system, followed by an inflammatory response which can include in more serious cases immune hyper-reactivity. Based on recent research from 2019, SARS-COV2 is likely to cause cell “pyroptosis” through the activation of the NLRP3 inflammasome. “Pyroptosis” is an inflammatory form of programmed cell death, meaning the cells are destroyed via an upregulation of inflammatory pathways involving various cytokines (inflammatory meditators or messengers), including IL-1β (Yang et al., 2020). The increased cell destruction allows debris and fluids to build up in the lungs leading to pneumonia and difficulty breathing in many cases.
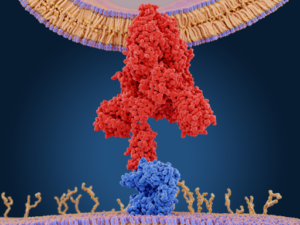
Viral Entry into Cells
It is believed that SARS-COV2 enters the cell via binding to a receptor known as ACE2. The ACE2 receptor is found on cells of different tissue types but primarily in endothelial or epithelial linings of the body, such as the vascular epithelium, lungs and gastrointestinal tract. It’s expressed at lower levels in the renal system and the central nervous system. The expression of the ACE2 receptor is part of an anti-inflammatory system, having anti-inflammatory effects throughout the body.
When damage to the endothelial or epithelial linings in your body takes place, your body increases the expression of ACE2, in order to activate this anti-inflammatory system. As a result, the people with the highest levels of ACE2 are people whose bodies are under stress and coping with inflammatory damage such as those with cardiovascular disease, high blood pressure, pulmonary disease, diabetes and smokers. Glycation (which causes damage to blood vessels from increased glucose levels) and high blood pressure (which causes forced damage to the lining of the blood vessels) lead to increased expression of the ACE2.
Unfortunately, ACE2 is the receptor this virus uses to enter our cells, so is the “gateway” to the cell, putting those with increased ACE2 receptors at increased risk of infection. This is the reason researchers believe that those with cardiovascular disease, pulmonary disease and diabetics and the elderly have increased risk of complications and death.
GI Connection
 Like SARS and MERS, SARS-COV2 also tends to infect the gastrointestinal tract in people who become ill. It is believed around a quarter of those infected develop a rather intense diarrhea. Early studies of this virus have found viral particles in stool samples which indicates it might also spread via feces (as SARS and MERS do). A new study just published in the American Journal of Gastroenterology showed that 30-48% of SARS-COV2 positive patients present with GI symptoms such as loose stool, diarrhea and abdominal cramping and those with diarrhea (28%) have a worse outcome. This supports the view that the virus can enter orally and replicate inside the gut.
Like SARS and MERS, SARS-COV2 also tends to infect the gastrointestinal tract in people who become ill. It is believed around a quarter of those infected develop a rather intense diarrhea. Early studies of this virus have found viral particles in stool samples which indicates it might also spread via feces (as SARS and MERS do). A new study just published in the American Journal of Gastroenterology showed that 30-48% of SARS-COV2 positive patients present with GI symptoms such as loose stool, diarrhea and abdominal cramping and those with diarrhea (28%) have a worse outcome. This supports the view that the virus can enter orally and replicate inside the gut.
Normally, viruses are destroyed by gastric acid produced by the stomach which acts as a protective barrier to infectious organisms entering the body via the mouth (GI tract). However, for those with decreased stomach acid production (ie: the elderly, people taking acid suppressing medication such as PPIs and those with H. pylori infection which suppresses acid production), they are at increased risk of viruses getting past the gastric barrier and migrating further down the GI tract where they can potentially breach the intestinal barrier and enter circulation. Chronic stress and “eating on the go” also decreases stomach acid production.
This data also raises the concern that those with pre-existing GI conditions such as inflammatory bowel disease, IBS (irritable bowel syndrome) or SIBO (small intestinal bacterial overgrowth) may be at increased risk of COVID-19 due to increased ACE2 receptors in the GI tract. To make matters worse, all of these conditions lead to gut permeability (leaky gut) which can allow viral entry into circulation leading to pulmonary infection. In other words, people with pre-existing GI conditions are at higher risk of both GI and pulmonary SARS-COV2 infection.
Immunity Against Viral Infections
 When the body encounters a viral infection, the immune system launches a number of specific and non-specific defense responses to eliminate the virus. The immune system synthesizes antibodies that bind to the virus and neutralize the virus while various types of T cells (lymphocytes) are produced to destroy the virus. Cytotoxic T cells, natural killer (NK) cells, and viral macrophages recognize and kill virus-infected cells via both specific and non-specific responses. Helper T cells can recognize virus-infected cells and produce a number of important cytokines which play important roles in fighting viral infections. However, in order for the immune system to work properly to fight against viral infections, there are a number of factors that come into play, such as age, pre-existing conditions, nutrient status, chronic stress (which suppresses immune responses), metabolic and hormone balance, environmental toxicity, sufficient sleep and lifestyle habits, such as smoking and physical activity.
When the body encounters a viral infection, the immune system launches a number of specific and non-specific defense responses to eliminate the virus. The immune system synthesizes antibodies that bind to the virus and neutralize the virus while various types of T cells (lymphocytes) are produced to destroy the virus. Cytotoxic T cells, natural killer (NK) cells, and viral macrophages recognize and kill virus-infected cells via both specific and non-specific responses. Helper T cells can recognize virus-infected cells and produce a number of important cytokines which play important roles in fighting viral infections. However, in order for the immune system to work properly to fight against viral infections, there are a number of factors that come into play, such as age, pre-existing conditions, nutrient status, chronic stress (which suppresses immune responses), metabolic and hormone balance, environmental toxicity, sufficient sleep and lifestyle habits, such as smoking and physical activity.
Populations at Risk
For 80-85% of the population, SARS-COV2 infections will remain relatively mild or non-existent. Most at risk are those over 85 years of age, who tend to have weaker immune systems and those with pre-existing cardiac, pulmonary and metabolic diseases, including diabetes. People with compromised immune systems or on immune-suppressive medication and smokers are also at increased risk. Based on recent research now emerging, gut health including having a healthy gut barrier and microbiome (gut bacteria), is paramount in one’s ability to fight viral infections and prevent risk of complications due to the important role these bacteria play in immune health.
Conventional Treatment
There currently is no FDA-approved drug or vaccination to treat or prevent COVID-19. There are a few drugs such as Remdesivir (antiviral), Favipiravir (antiviral), Methylene blue (antimalarial), azithromycin (antibiotic), tocilizumab (monoclonal antibody) and chloroquine (an old antimalarial drug) which seem to show some promise as potential treatments, but FDA-approval for these drugs are not to be expected soon. Drugs and vaccines for new organisms usually take a year or more to develop.
The Functional Medicine Approach to Viral Infection
In Functional Medicine, we emphasize the importance of developing and maintaining immune resistance to:
- Reduce risk of infection
- Minimize symptoms, promote immune defenses and prevent complications
Functional Medicine takes a comprehensive approach to the prevention and management of viral infections. This includes addressing any current immune challenges or chronic inflammation which may inhibit a robust immune response to any new viral exposure. We address all aspects of a patient’s health and lifestyle that impacts risk of infection and ability to fend off a viral attack.
Gut Immune Defense
The first defense against viral infections is a healthy immune response. Since about 70-80% of your immune system is located in your GI tract, a healthy gut lining where these immune cells reside and a well-balanced gut flora that interact with these immune cells and protect our GI tract against pathogens, play a critical role in immune defense.
Antibodies (called “secretory IgA”) are produced by immune cells in the intestinal lining which protect the body from various pathogens and toxic compounds in the gut. The health of the gastrointestinal tract is critical to overall immune health.
Diet, Nutrition and Lifestyle
 Diet plays an important role in immune health.
Diet plays an important role in immune health.
- A plant-based high-fiber diet rich in fruit, vegetables, legumes, nuts and seeds together with fish and seafood, has been shown to improve both gut and immune health
- A processed food diet high in sugars and processed fats diminishes immune health.
Lifestyle habits are critical for immune health:
- Adequate sleep is crucial to allow our immune system to rejuvenate
- Regular physical exercise is essential to maintain immune health
- Stress management is important as chronic stress suppresses immune responses
- Minimizing exposure to environmental toxins, cigarette smoke and heavy metals also interfere with the immune system
Anti-Viral Nutrients and Botanicals
 The immune system, like any other system in the body, requires a wide variety of vitamins, minerals and other nutrients to function optimally. Vitamin A, vitamin C, vitamin D, N-acetylcysteine or glutathione, zinc, selenium, and essential fatty acids appear to be the most important to maintain immune health and fight viral infection. In addition, there are a number of herbs that have been shown to have antiviral effects by either preventing viral binding to cells, blocking viral replication or having direct antiviral effects. In addition, many herbs have been shown to improve immune responses against viruses, have antioxidant or anti-inflammatory effects or promote cell function in other ways.
The immune system, like any other system in the body, requires a wide variety of vitamins, minerals and other nutrients to function optimally. Vitamin A, vitamin C, vitamin D, N-acetylcysteine or glutathione, zinc, selenium, and essential fatty acids appear to be the most important to maintain immune health and fight viral infection. In addition, there are a number of herbs that have been shown to have antiviral effects by either preventing viral binding to cells, blocking viral replication or having direct antiviral effects. In addition, many herbs have been shown to improve immune responses against viruses, have antioxidant or anti-inflammatory effects or promote cell function in other ways.
Based on extensive published literature and a detailed evaluation of the physical status of the patient, possible strategies of herbal and nutritional intervention may include:
- Blocking viral acquisition/entry and supporting mucosal defenses (ie: vitamin A, vitamin D, essential fatty acids, glutamine, licorice, elderberry, oregano oil, Chinese skullcap, aloe vera, probiotics, zinc)
- Targeting viruses directly (ie: licorice, astragalus, elderberry, andrographis, artemisinin, olive leaf, garlic, thuja occidentalis, Japanese honesuckle, Chinese skullcap, St. John’s wort, zinc, silver hydrosol)
- Blocking viral replication (ie: licorice, elderberry, berberine, zinc, selenium, NAC, silver hydrosol)
- Supporting immune function/NK activity, Th1 responses (ie: vitamin A, vitamin C, vitamin D, echinacea, astragalus, cordyceps, rhodiola, eleuthero, licorice, aloe vera, elderberry, NAC, glutathione, glutamine, zinc)
- Decreasing oxidative stress, inflammation and inflammatory by-products of viruses, such as histamine (vitamin C, vitamin E, selenium, NAC, glutathione, zinc, turmeric, resveratrol, grape seed extract, green tea, olive leaf, milk thistle, elderberry and berberine)
- Supporting cell function (ie: B vitamins, vitamin D, magnesium, NAC, glutathione, CoQ10, berberine, essential fatty acids and phospholipids)
Vitamin A
 Efficacy against a wide-range of bacterial and viral infections
Efficacy against a wide-range of bacterial and viral infections- Essential for normal immune function, growth, development and maintenance of epithelial cells (GI tract)
- Subclinical deficiency results in increased susceptibility to common infectious disease (WHO)
- High doses are recommended by WHO and UNICEF in a joint statement for all children with measles in communities where vitamin A deficiency is a recognized problem
Vitamin A deficiency impairs innate immunity by impeding normal regeneration of mucosal epithelial barriers (ie: pulmonary and gut barriers) damaged by infection, and by diminishing the function of various white blood cells and natural killer (NK) cells needed to fight viruses. Vitamin A is also required for adaptive immunity and plays a role in the development of both T-helper (Th) cells and B-cells. Vitamin A deficiency diminishes both Th2-directed antibody-mediated responses and Th1-mediated immunity. These changes in mucosal epithelial regeneration and immune function presumably account for the increased mortality seen in vitamin A-deficient infants, young children, and pregnant women in many third world countries.
Vitamin C
- Anti-viral agent
- Important antioxidant and immune stimulant
- Shortens duration and severity of symptoms of the flu and common cold
- Breaks down histamine and so has anti-histamine function
 Most of the world, especially Asia and continental Europe, recognize Vitamin C as an important anti-viral agent. It is an important antioxidant and is vital to the function of leukocytes (white blood cells that help to fight infections) and overall immune system health. Many studies have established the antiviral effects of vitamin C against many viruses, especially influenza and the common cold. Studies have shown that the duration of the common cold was frequently shorter and less severe among people with sufficient vitamin C levels. Vitamin C also may also protect against infection caused by coronavirus. Three human controlled trials have reported that there was significantly lower incidence of pneumonia in vitamin C‐supplemented groups, suggesting that vitamin C might prevent the susceptibility to lower respiratory tract infections.
Most of the world, especially Asia and continental Europe, recognize Vitamin C as an important anti-viral agent. It is an important antioxidant and is vital to the function of leukocytes (white blood cells that help to fight infections) and overall immune system health. Many studies have established the antiviral effects of vitamin C against many viruses, especially influenza and the common cold. Studies have shown that the duration of the common cold was frequently shorter and less severe among people with sufficient vitamin C levels. Vitamin C also may also protect against infection caused by coronavirus. Three human controlled trials have reported that there was significantly lower incidence of pneumonia in vitamin C‐supplemented groups, suggesting that vitamin C might prevent the susceptibility to lower respiratory tract infections.
A placebo-controlled trial involving 715 students between the ages 18-32 taking 1,000 mg four times daily found an 85% decrease in flu and cold symptoms compared to the control. Keep in mind approximately 15-30% of upper respiratory tract infections involve coronaviruses so there is a good chance it helps protect against coronaviruses.
Higher intakes of vitamin C may potentially help people who are critically ill with COVID-19 and on ventilators. A review of several studies performed prior to the emergence of COVID-19 found a dose of 1,000 to 6,000 mg of vitamin C daily (intravenously or by mouth) shortened the time on ventilation by about 25% for people who required ventilation for over 10 hours, but it appeared to be less helpful for those on ventilators for shorter periods.
At this moment, China is conducting several clinical trials with intravenous Vitamin C to now actively treating patients with intravenous Vitamin C. A trial at Zhongnan Hospital in Wuhan is using 24,000 mg per day intravenously. The Shanghai Medical Association has released an expert consensus statement on the comprehensive treatment of COVID-19 where they endorse the use of high-dose IV vitamin C for the illness. Vitamin C also helps to breakdown and reduce histamine produced by viral infections which causes symptoms such as sneezing, runny nose, nasal congestion and is immuno-suppressive
Vitamin D
 Enhances vitamin A function
Enhances vitamin A function- Improves gut barrier function
- Enhances both specific and non-specific innate immunity in a wide range of viral infections including HIV, HPV, hepatitis
- Reduces systemic inflammation, neuroinflammation
- Improves mitochondrial function and muscle strength
Vitamin D deficiency is associated with an increased risk in autoimmunity illnesses and greater susceptibility to infection. It also supports the body’s mucosal defenses which are critical for protecting ourselves from infectious respiratory viruses. Vitamin D supplements, taken daily in moderate doses, helps to reduce the risk of respiratory infections and viruses such as influenza A in children and adults who are deficient (< 20 ng/mL) or severely deficient (< 10 ng/mL) in vitamin D.
Harvard and Massachusetts General Hospital in conjunction with a global collaborative study following up on a Cochrane analysis of 25 randomized controlled trials involving 11,000 participants confirmed that vitamin D taken daily or weekly significantly cut the risk of respiratory infections in half. Efficacy was shown in a wide range of viral respiratory infections.
A 2018 meta-analysis study concluded vitamin-D deficiency may confer increased susceptibility to enveloped viral infections such as HIV, Hepatitis, Dengue and Respiratory Syncytial virus infection, among others.
A 2011 narrative review concluded that interventional and observational epidemiological studies provide evidence that vitamin D deficiency may confer increased risk of influenza and respiratory tract infection. Vitamin D deficiency is also prevalent among patients with HIV infection. Cell culture experiments support the thesis that vitamin D has direct anti-viral effects particularly against enveloped viruses.
A meta-analysis and systematic review from Children’s Hospital of Philadelphia identified 13 of 18 studies confirming that Vitamin D protected against acute respiratory infection. Since coronaviruses causes 15-30% of upper respiratory infections, vitamin D likely helps protect against coronaviral infection.
A randomized double-blind placebo trial to measure the rate that Vitamin D reduced seasonal influenza A conducted in Japan found almost twice as many participants in the placebo group came down with the flu compared to the vitamin D group. The Japanese scientists also observed that people with a history of asthma were best protected.
Zinc
 Reduces severity and duration of common cold symptoms
Reduces severity and duration of common cold symptoms- Inhibits viral replication by blocking RNA polymerase activity
- Reduces mortality for a wide range of infectious diseases
- Provides antioxidant benefits
- Important for gut barrier function
Many different cell types of the innate immune system, comprising dendritic cells (DCs), mast cells, monocytes/macrophages, natural killer (NK) cells, as well as in the adaptive immune system, comprising T-cells and B-cells rely on zinc signaling. A variety of studies carried out in humans and animals indicate suppressed immune responses as a result of zinc deficiency, accompanied by increased susceptibility to a multitude of infectious agents, including HIV, malaria and the common cold.
Zinc supplementation is repeatedly shown to reduce mortality for a wide range of infectious diseases. A Cochrane analysis revealed that zinc supplementation within 24 hours of the onset of common cold symptoms reduced the severity and duration in otherwise healthy people. Moreover, zinc supplementation for at least 5 months showed beneficial effects in terms of reduced cold incidence, less school absence, and lower intake of antibiotics.
Zinc inhibits coronavirus and RNA polymerase activity in vitro and zinc ionophores (which allow zinc to enter the cell) have been shown to block replication of these RNA viruses in cell culture. This is currently the believed mechanism of action of how the antimalarial drugs chloroquine and hydroxychloroquine inhibit viral replication: by acting as zinc ionophores to allow zinc to enter the cell.
Zinc provides antioxidant benefits by functioning as a cofactor for the antioxidant superoxide dismutase (SOD) enzyme and helps to improve gut barrier function, decreasing risk of infectious disease.
Selenium
- Functions to reduce viral replication and viral mutation
- Provides anti-inflammatory and antioxidant effects
- Increases glutathione (GSH) levels
Selenium is required for proper development and functioning of all different types of leukocytes (white blood cells) of the immune system. Selenium metabolites can have significant effects on macrophage activation, differentiation, and function. Low selenium status can reduce phagocytic capacity, superoxide production, and cytokine secretion by macrophages (Safir et al., 2003)
Effective antiviral immunity requires effective cell-mediated immunity and in many cases strong neutralizing antibodies produced through the humoral immune response. While selenium research has not focused on the coronavirus, studies have shown selenium increases T-cell responses to poliovirus and improves poliovirus clearance (Broome et al., 2004). In selenium deficiency, benign strains of Coxsackievirus and influenza virus can mutate to highly pathogenic strains leading to Keshan disease (Beck, 1997). Keshan disease in parts of China has been shown to be fully preventable with selenium supplementation. Selenium status or deficiencies may affect many other viral infections including influenza, HIV, IAV, hepatitis C virus, poliovirus and West Nile virus (Steinbrenner et al. 2015). In HIV infections, selenium status can influence the course of infection, and the infection can affect the selenium status of the individual (Baum et al., 1997).
N-Acetyl-Cysteine (NAC)
 Direct and indirect antioxidant
Direct and indirect antioxidant- Increases production of glutathione (GSH)
- Supports phase II conjugation and protects the liver
- Anti-inflammatory and inhibits replication of influenza A
- Mucolytic
- Disrupts biofilms
Oxidative stress is a well-known pathway for microbial infections such as viruses and bacterial pneumonia, especially in the lungs. When the lungs are subject to serious oxidative stress, there is an increase in inflammatory cytokines, especially IL-1, IL-8 and tumor necrosis factor-alpha (TNFa). Each of these cytokines have been shown repeatedly in clinical research to play a role in different respiratory infections including influenza, coronavirus, echovirus, adenovirus, coxsackie virus and others. Therefore, certain antioxidants can alleviate lung damage due to oxidative stress. N-acetyl cysteine is one of these extremely important antioxidants.
NAC exhibits both direct and indirect antioxidant properties. The indirect benefit is that it increases the concentration of another important antioxidant, glutathione, in the lung cells. There is no confirmatory evidence that NAC directly targets influenza or flu-like viral infections, however, it has been shown to inhibit viral replication and significantly reduce the rate of clinical symptoms.
Johann Goethe University Department of Virology observed that NAC inhibits the replication of seasonal human influenza A viruses by decreasing several of these pro-inflammatory molecules. The scientists recommend that NAC should be included as an additional treatment option in the case of an influenza A pandemic.
An Italian randomized placebo study conducted at the University of Genoa found that subjects who were already suspected of having contact with the H1N1 flu virus who were placed under NAC treatment had a 25% rate of experiencing symptoms compared to 79% in the placebo group.
Glutathione (GSH)
- Critical intracellular antioxidant
- Regulates both innate and adaptive immune responses
- Regulates NK cell activity
- Helps balance Th1 and Th2 activity
 Glutathione, which is a tripeptide antioxidant with a crucial role in reducing oxidative stress and protecting the cell and the mitochondria against a wide range of toxins, also has a wide-ranging role in immunity. Its functions affect essentially every cell of the immune system and has important effects on both innate and adaptive immunity. In the innate immune system, GSH enhances the cytotoxic and antimicrobial effects of nitric oxide (NO) used by phagocytic cells.
Glutathione, which is a tripeptide antioxidant with a crucial role in reducing oxidative stress and protecting the cell and the mitochondria against a wide range of toxins, also has a wide-ranging role in immunity. Its functions affect essentially every cell of the immune system and has important effects on both innate and adaptive immunity. In the innate immune system, GSH enhances the cytotoxic and antimicrobial effects of nitric oxide (NO) used by phagocytic cells.
Natural killer (NK) cells act as cytotoxic lymphocytes and have wide ranging antimicrobial and antiviral activity. NK function is directly dependent on GSH in the cells. GSH depletion in NK cells significantly diminishes the ability of NK cells to destroy pathogens. In addition, increasing GSH levels in NK cells in healthy subjects increases the ability of NK cells to recognize microbes and respond accordingly.
In the adaptive immune system, GSH helps to maintain balance between T helper 1 (Th1) and T helper 2 (Th2) responses. T helper cells are regulators of the type of adaptive response the immune system will develop. In viral infections, a Th1 response should predominate with an increase in proinflammatory cytokines. GSH deficiency or depletion appears to decrease production of proinflammatory cytokines while redirecting the immune system to a Th2-mediated response, one poorly suited for dealing with intracellular invasion.
HIV infection diminishes the ability of GSH to restore homeostasis. HIV infection leads to massive free radical production in the body, depleting the levels of GSH and maintaining a state of oxidative stress. It appears that decreasing the levels of GSH in immune cells is a powerful mechanism by which bacteria and viruses have evolved to avoid the effector mechanisms of the immune system. Compromised levels of intracellular GSH aid these microbes in surviving intracellularly through a multitude of mechanisms. GSH allows for increased control of intracellular infections through its influence on cells of the innate immune system. GSH supplementation has immune-stimulating effects in T-cells, leading to improved control of various infections.
Licorice Root (Glycyrrhiza glabra)
 For thousands of years, in traditional Chinese medicine (TCM) and other traditional medicines, licorice root has been used to treat ulcers, sore throats, bronchitis, coughs, adrenal insufficiencies and allergic diseases. Ancient manuscripts from China, India and Greece all include licorice for treating respiratory tract infections and hepatitis. Licorice root’s main antiviral compounds are known as ‘glycyrrhizins’.
For thousands of years, in traditional Chinese medicine (TCM) and other traditional medicines, licorice root has been used to treat ulcers, sore throats, bronchitis, coughs, adrenal insufficiencies and allergic diseases. Ancient manuscripts from China, India and Greece all include licorice for treating respiratory tract infections and hepatitis. Licorice root’s main antiviral compounds are known as ‘glycyrrhizins’.
For the last 20 years, glycyrrhizins have been used intravenously to treat chronic hepatitis B and C infections with very rare side effects. It has also been shown to directly inhibit replication of SARS-associated coronavirus and inhibits binding and penetration of the virus. Glycyrrhizins show activity against a wide variety of viruses including HIV, herpes virus, hepatitis and influenza and many other RNA and DNA viruses. Glycyrrhizin has also been used to treat patients with HIV-1 and chronic hepatitis C virus.
A 2003 study compared the antiviral effects of glycyrrhizin on two isolates of coronavirus from patients with SARS admitted to the clinical center of Frankfurt University, Germany, to four other widely-used medications known to have antiviral, anti-tumor, and immunosuppressive activity. They found that glycyrrhizin was the most potent inhibitor of SARS-CV replication in cells. In addition to inhibition of virus replication, glycyrrhizin inhibited binding and penetration of the virus. The researchers concluded:
“Of all the compounds, glycyrrhizin was the most effective in inhibiting replication of the SARS-associated virus. Our findings suggest that glycyrrhizin should be assessed for treatment of SARS.” (Lancet, 2003)
Astragalus (Astragalus membranaceus)
 Astragalus is another herb used for thousands of years in both TCM and Ayurvedic medicine for lung health and upper respiratory infection. The compounds found in astragalus (saponins) have been well researched and found to inhibit influenza proliferation. Jinlin Academy of Agricultural Sciences in China conducted a study that concluded “Astragalus exhibits antiviral properties that can treat infectious bronchitis caused by [avian] coronavirus”.
Astragalus is another herb used for thousands of years in both TCM and Ayurvedic medicine for lung health and upper respiratory infection. The compounds found in astragalus (saponins) have been well researched and found to inhibit influenza proliferation. Jinlin Academy of Agricultural Sciences in China conducted a study that concluded “Astragalus exhibits antiviral properties that can treat infectious bronchitis caused by [avian] coronavirus”.
The USDA’s Avian Disease and Oncology Laboratory found astragalus inhibits avian flu viruses and has been studied in several avian infections. Beijing University of Chinese Medicine recently completed an analysis of previous research looking at the benefits of Chinese herbal formulas against the SARS coronavirus and H1N1 flu (swine flu). In 3 studies, among participants who took formulas against SARS, none contracted the illness. Nor did any contract H1N1 influenza in four additional studies. A primary ingredient in these formulas was astragalus.
The prestigious journal Science recently published a review out of Yun-nan Academy of Agricultural Sciences in China that investigated the large disparities in infection and mortality rates between different provinces, Wuhan being the most severe. In the provinces with the lowest infection rates, there was between an 84% to 98% use of TCM formulas. Again, two of the main ingredients were astragalus and ginseng.
Research on astragalus suggests that it blocks several TLRs (the receptors that indicate danger to your immune system and launch the inflammatory pathway). One of the components of astragalus, astragaloside IV, is also cardioprotective.
Elderberry (Sambucus nigra)
 There have been two small clinical trials that demonstrate that elderberry extract shortens the length of infection when compared to placebo by four days. Hadassah University Hospital in Israel found that elderberry was effective in vitro against 10 different influenza strains with improvements in cytokine profiles confirming its anti-inflammatory and antiviral properties.
There have been two small clinical trials that demonstrate that elderberry extract shortens the length of infection when compared to placebo by four days. Hadassah University Hospital in Israel found that elderberry was effective in vitro against 10 different influenza strains with improvements in cytokine profiles confirming its anti-inflammatory and antiviral properties.
A 2019 study observed that certain compounds in elderberry inhibit the flu virus’s entry and replication in human cells. In 2014, researchers at Emory University noted that elderberry extract inhibited coronavirus activity at the point of infection and the researchers hypothesized that elderberry rendered the virus non-infectious. Elderberry appears to affect lipid rafts, which means that it can inhibit viral uptake and viral budding (preventing infection). This is a mechanism that would make elderberry important for any viral infection, including SARS-COV2.
Contrary to some initial concerns, elderberry does not stimulate a cytokine storm in any research study. In fact, elderberry can reduce reactive oxygen species (ROS) and inflammatory cytokine secretion by blocking NF-kB pathways. The lack of reports of cytokine storm is significant considering that a few clinical trials have been completed.
Echinacea (Echinacea purpurea)
 Echinacea appears to have broad antiviral effects. It has been shown to prevent influenza A, avian flu, and swine flu and have activity against herpes simplex 1 and 2 in vitro. Echinacea can kill HIV-1 by blocking the enzyme that allows it to integrate its genetic material into the host cell. A 2012 review of the research on echinacea found that it had multiple immune-modulatory effects, including stimulation of certain immune activity such as phagocytic activity of macrophages and suppression of the proinflammatory responses of epithelial cells to viruses, which makes it an ideal antiviral agent. The review article also found:
Echinacea appears to have broad antiviral effects. It has been shown to prevent influenza A, avian flu, and swine flu and have activity against herpes simplex 1 and 2 in vitro. Echinacea can kill HIV-1 by blocking the enzyme that allows it to integrate its genetic material into the host cell. A 2012 review of the research on echinacea found that it had multiple immune-modulatory effects, including stimulation of certain immune activity such as phagocytic activity of macrophages and suppression of the proinflammatory responses of epithelial cells to viruses, which makes it an ideal antiviral agent. The review article also found:
“All strains of human and avian influenza viruses tested (including a Tamiflu-resistant strain), as well as herpes simplex virus, respiratory syncytial virus, and rhinoviruses, were very sensitive to a standardized Echinacea purpurea preparation”.
Echinacea appears to modify the clinical course of flu-like respiratory infection by increasing cytokine and phagocytic activity to fight viral infection. A 2012 double-blind study which examined whether echinacea provided protection to air travelers concluded:
“Supplementation with standardized Echinacea tablets, if taken before and during travel, may have preventive effects against the development of respiratory symptoms during travel involving long-haul flights.”
One of the largest double-blind, placebo-controlled studies on echinacea followed participants for four months and confirmed the safety of long term echinacea supplementation. It also observed a statistically significant decrease in cold episodes in the echinacea group. Since coronavirus causes 15-30% of upper respiratory infections, it is likely echinacea likely helps against coronavirus.
Olive Leaf (Olea europaea)
 In 1969 researchers demonstrated olive leaf constituents are powerful in vitro inhibitors of numerous viruses, including parainfluenza, herpes, pseudorabies, and some forms of polio. Nearly every virus studied, including several cold and influenza viruses, was inactivated when exposed to a constituent of OLE, calcium elenolate. More recently, olive leaf extract was shown to be effective against HIV, inhibiting its replication. Olive leaf also prevents viral infectivity by inhibiting assembly at the cell membrane, stopping viral shedding.
In 1969 researchers demonstrated olive leaf constituents are powerful in vitro inhibitors of numerous viruses, including parainfluenza, herpes, pseudorabies, and some forms of polio. Nearly every virus studied, including several cold and influenza viruses, was inactivated when exposed to a constituent of OLE, calcium elenolate. More recently, olive leaf extract was shown to be effective against HIV, inhibiting its replication. Olive leaf also prevents viral infectivity by inhibiting assembly at the cell membrane, stopping viral shedding.
Since then, the majority of the studies on OLE have focused on its anti-inflammatory and antioxidant effects rather than its antiviral activity against viral upper respiratory infections. Still, there is considerable evidence to support olive leaf’s ability to strengthen the immune system against other infectious viral diseases in addition to possessing many anti-inflammatory and antioxidant qualities.
One randomized trial performed by the University of Auckland in New Zealand suggests olive leaf can contribute to treating respiratory illnesses, including coronavirus. A 2001 study out of the University of Hong Kong identified 6 separate antiviral agents in olives that were effective against parainfluenza and respiratory syncytial virus (RSV).
A 2019 study on 32 high school athletes found that OLE supplementation over a season did not significantly reduce incidence of upper respiratory tract infection, but did decrease duration of sick days by 28%.
A 2005 in vitro study on the antiviral effects of oleuropein derived from olive leaf against an enveloped salmonid rhabdovirus fount that it inhibited the in vitro infectivity of the viral hemorrhagic septicemia virus (VHSV) suggesting interactions with the viral envelope. The researchers concluded:
“Therefore, we propose that O. europaea could be used as a potential source of promising natural antivirals, which have demonstrated to lack [negative] impact on health and environment. In addition, OLE could be used to design other related antiviral agents.”
Oregano Oil (Origanum vulgare)
 Oregano possesses a compound called carvacrol that has been shown to have broad-range antibacterial and antiviral effects, as well as antioxidant and anticancer activities. It is particularly effective against bacterial food‐borne pathogens, including Escherichia coli, Salmonella, and Bacillus cereus. Oregano oil has shown partial efficacy against respiratory syncytial virus, coxsackie virus B3, and HSV1.
Oregano possesses a compound called carvacrol that has been shown to have broad-range antibacterial and antiviral effects, as well as antioxidant and anticancer activities. It is particularly effective against bacterial food‐borne pathogens, including Escherichia coli, Salmonella, and Bacillus cereus. Oregano oil has shown partial efficacy against respiratory syncytial virus, coxsackie virus B3, and HSV1.
A 2005 animal study examined efficacy of vapors of oregano oil and fount it to be effective against acute otitis media caused by pneumococci or H. influenzae, healing 56–81% of rats infected with H. influenzae and 6–75% of rats infected with pneumococci, compared with 5.6–6% of rats in the placebo group.
A 2010 study focused on oregano’s antiviral properties against influenza virus. Although oregano did not kill the virus it nevertheless inhibited the virus’ ability to translate proteins responsible for viral binding to cells.
Berberine
In vitro studies show berberine from barberry, goldenseal and Oregon grape root, decreases production of inflammatory cytoki nes such as TNF-alpha and IL-6. Animal studies of influenza show evidence that berberine reduces inflammation through inhibition of various inflammatory pathways, including the NF-kB, pathway. It also decreases production of HIV proteases at the level of protein production, acting as a protease inhibitor. Berberine reduces viral replication of respiratory syncytial virus (RSV) and reduces IL-6 mRNA, suggesting that it reduces inflammation. Together these studies suggest that berberine could inhibit SARS-CoV2 infection – although it hasn’t been studied specifically for SARS-CoV2.
nes such as TNF-alpha and IL-6. Animal studies of influenza show evidence that berberine reduces inflammation through inhibition of various inflammatory pathways, including the NF-kB, pathway. It also decreases production of HIV proteases at the level of protein production, acting as a protease inhibitor. Berberine reduces viral replication of respiratory syncytial virus (RSV) and reduces IL-6 mRNA, suggesting that it reduces inflammation. Together these studies suggest that berberine could inhibit SARS-CoV2 infection – although it hasn’t been studied specifically for SARS-CoV2.
Summary of the Functional Medicine Approach to Viral Infection
- Optimize intestinal lining health and gut flora balance
- Adopt a plant-based diet rich in fruits and vegetables and fish and seafood, avoiding meat and processed meat and all over processed foods
- Optimize intake of immune-support nutrients (vitamins A, C, E, zinc, selenium, NAC, etc.)
Ensure adequate sleep and exercise - Minimize stress
- Avoid environmental toxins, cigarettes and heavy metals (including dental amalgams)
- Consider antiviral herbs for prevention or management of viral infection (consult with herbalist for best results)
References
Yang, Y., Peng, F., Wang, R., Guan, K., Jiang, T., Xu, G., Sun, J., & Chang, C. (2020). The deadly coronaviruses: The 2003 SARS pandemic and the 2020 novel coronavirus epidemic in China. Journal Of Autoimmunity, 102434. https://doi-org.uws.idm.oclc.org/10.1016/j.jaut.2020.102434
Rothan, H. A., & Byrareddy, S. N. (2020). The epidemiology and pathogenesis of coronavirus disease (COVID-19) outbreak. Journal of Autoimmunity. https://doi-org.uws.idm.oclc.org/10.1016/j.jaut.2020.102433
Bertram S, Heurich A, Lavender H, Gierer S, Danisch S, Perin P, et al. (2012) Influenza and SARS-Coronavirus Activating Proteases TMPRSS2 and HAT Are Expressed at Multiple Sites in Human Respiratory and Gastrointestinal Tracts. PLoS ONE 7(4): e35876. https://doi.org/10.1371/journal.pone.0035876
Study from The American Journal of Gastroenterology Reveals Diarrhea is a Prominent Symptom of COVID-19. (2020). PR Newswire.
Zhang, L, Liu, Y. Potential interventions for novel coronavirus in China: A systematic review. J Med Virol. 2020; 92: 479– 490. https://doi.org/10.1002/jmv.25707
Stephensen, C. B. (2001). Vitamin A, Infection, and Immune Function*. Annual Review of Nutrition, 21(1), 167.
Hemila H. Vitamin C and SARS coronavirus. J Antimicrob Chemother. 2003;52:1049‐1050.
Field CJ, Johnson IR, Schley PD. Nutrients and their role in host resistance to infection. J Leukoc Biol. 2002;71:16‐32.
Hemila H. Vitamin C intake and susceptibility to pneumonia. Pediatr Infect Dis J. 1997;16:836‐837.
Calder, P. C., & Kulkarni, A. D. (2018). Nutrition, Immunity, and Infection. CRC Press.
Laplana, M., Royo, J. L., & Fibla, J. (2018). Vitamin D Receptor polymorphisms and risk of enveloped virus infection: A meta-analysis. Gene, 678, 384–394. https://doi-org.uws.idm.oclc.org/10.1016/j.gene.2018.08.017
Beard, J. A., Bearden, A., & Striker, R. (2011). Vitamin D and the anti-viral state. Journal of Clinical Virology, 50(3), 194–200. https://doi-org.uws.idm.oclc.org/10.1016/j.jcv.2010.12.006
Pilcher, H. Liquorice may tackle SARS. Nature (2003). https://doi.org/10.1038/news030609-16
Cinatl, J., Morgenstern, B., Bauer, G., Chandra, P., Rabenau, H., & Doerr, H. W. (2003). Glycyrrhizin, an active component of liquorice roots, and replication of SARS-associated coronavirus. Lancet, 361(9374), 2045–2046. https://doi-org.uws.idm.oclc.org/10.1016/S0140-6736(03)13615-X
Astragalus polysaccharides enhance the immune response to avian infectious bronchitis virus vaccination in chickens. – PubMed – NCBI. https://www-ncbi-nlm-nih-gov.liboff.ohsu.edu/pubmed/28826771. Accessed March 21, 2020.
Astragalus polysaccharides inhibit avian infectious bronchitis virus infection by regulating viral replication. – PubMed – NCBI. https://www-ncbi-nlm-nih-gov.liboff.ohsu.edu/pubmed/29170045. Accessed March 21, 2020.
Liu T, Zhang M, Niu H, et al. Astragalus polysaccharide from Astragalus Melittin ameliorates inflammation via suppressing the activation of TLR-4/NF-κB p65 signal pathway and protects mice from CVB3-induced virus myocarditis. Int J Biol Macromol. 2019;126:179-186. doi:10.1016/j.ijbiomac.2018.12.207
Liang Y, Zhang Q, Zhang L, Wang R, Xu X, Hu X. Astragalus Membranaceus Treatment Protects Raw264.7 Cells from Influenza Virus by Regulating G1 Phase and the TLR3-Mediated Signaling Pathway. Evid-Based Complement Altern Med ECAM. 2019;2019. doi:10.1155/2019/2971604
Hsieh H-L, Liu S-H, Chen Y-L, Huang C-Y, Wu S-J. Astragaloside IV suppresses inflammatory response via suppression of NF-κB, and MAPK signalling in human bronchial epithelial cells. Arch Physiol Biochem. February 2020:1-10. doi:10.1080/13813455.2020.1727525
Wang, Xiaoguang & Liu, Zejing. (2014). Prevention and treatment of viral respiratory infections by traditional Chinese herbs. Chinese medical journal. 127. 1344-50. 10.3760/cma.j.issn.0366-6999.20132029.
Elderberry for Influenza | The Medical Letter, Inc. https://secure-medicalletter-org.liboff.ohsu.edu/w1566f. Accessed March 21, 2020.
Zakay-Rones Z, Varsano N, Zlotnik M, et al. Inhibition of several strains of influenza virus in vitro and reduction of symptoms by an elderberry extract (Sambucus nigra L.) during an outbreak of influenza B Panama. J Altern Complement Med N Y N. 1995;1(4):361-369. doi:10.1089/acm.1995.1.361
Zakay-Rones Z, Thom E, Wollan T, Wadstein J. Randomized study of the efficacy and safety of oral elderberry extract in the treatment of influenza A and B virus infections. J Int Med Res. 2004;32(2):132-140. doi:10.1177/147323000403200205
Shahsavandi S, Ebrahimi MM, Hasaninejad Farahani A. Interfering With Lipid Raft Association: A Mechanism to Control Influenza Virus Infection By Sambucus Nigra. Iran J Pharm Res IJPR. 2017;16(3):1147-1154.
Lin P, Hwang E, Ngo HTT, Seo SA, Yi T-H. Sambucus nigra L. ameliorates UVB-induced photoaging and inflammatory response in human skin keratinocytes. Cytotechnology. 2019;71(5):1003-1017. doi:10.1007/s10616-019-00342-1
Manayi A, Vazirian M, Saeidnia S. Echinacea purpurea: Pharmacology, phytochemistry and analysis methods. Pharmacogn Rev. 2015;9(17):63-72. doi:10.4103/0973-7847.156353
Hudson, J. B. (2012). Applications of the phytomedicine Echinacea purpurea (Purple Coneflower) in infectious diseases. Journal Of Biomedicine & Biotechnology, 2012, 769896. https://doi-org.uws.idm.oclc.org/10.1155/2012/769896
Brinker, F. (2008). Echinacea for Upper Respiratory Viral Infections: Preparatory Differences Matter. Alternative Medicine Alert, 11(4), 41–45.
Rajabiesterabadi, H., Ghelichi, A., Jorjani, S., Hoseini, S. M., & Akrami, R. (2020). Dietary olive (Olea europaea) leaf extract suppresses oxidative stress and modulates intestinal expression of antioxidant- and tight junction-related genes in common carp (Cyprinus carpio). Aquaculture, 520. https://doi-org.uws.idm.oclc.org/10.1016/j.aquaculture.2019.734676
Somerville, V., Moore, R., & Braakhuis, A. (2019). The Effect of Olive Leaf Extract on Upper Respiratory Illness in High School Athletes: A Randomised Control Trial. Nutrients, 11(2), 358. https://doi-org.uws.idm.oclc.org/10.3390/nu11020358
Olive Leaf. (2009). Alternative Medicine Review, 14(1), 62–66.
Renis HE. In vitro antiviral activity of calcium elenolate. Antimicrob Agents Chemotber (Bcthesda) 1969:9:167-172.
Lee-Huang S, Zhang L, Huang PL, et al. Anti-HIV activity of olive leaf extract (OLE) and modulation of host cell gene expression by HIV-1 infection and OLE treatment. Biocheni Biophys Res Commun 2003:307:1029-1037.
Micol V, Caturla N, Pérez-Fons L, et al. The olive leaf extract exhibits antiviral activity against viral haemorrhagic septicaemia rhabdovirus (VHSV). AHííVir.i/Ri-s 2005;66:129-136.
Wu, S., Patel, K. B., Booth, L. J., Metcalf, J. P., Lin, H. K., & Wu, W. (2010). Protective essential oil attenuates influenza virus infection: an in vitro study in MDCK cells. BMC complementary and alternative medicine, 10, 69. https://doi.org/10.1186/1472-6882-10-69
Zhang X-L, Guo Y-S, Wang C-H, et al. Phenolic compounds from Origanum vulgare and their antioxidant and antiviral activities. Food Chem. 2014;152:300-306. doi:10.1016/j.foodchem.2013.11.153
Sharifi, R. M., Varoni, E. M., Iriti, M., Martorell, M., Setzer, W. N., del Mar Contreras, M., Salehi, B., Soltani, N. A., Rajabi, S., Tajbakhsh, M., Sharifi, R. J., Sharifi-Rad, M., Soltani-Nejad, A., & Sharifi-Rad, J. (2018). Carvacrol and human health: A comprehensive review. Phytotherapy Research, 32(9), 1675.
Kristinsson, K. G., Magnusdottir, A. B., Petersen, H., & Hermansson, A. (2005). Effective treatment of experimental acute otitis media by application of volatile fluids into the ear canal. The Journal of Infectious Diseases, 191(11), 1876–1880.
Zha W, Liang G, Xiao J, et al. Berberine Inhibits HIV Protease Inhibitor-Induced Inflammatory Response by Modulating ER Stress Signaling Pathways in Murine Macrophages. PLoS ONE. 2010;5(2). doi:10.1371/journal.pone.0009069
Anti‐influenza activity of berberine improves prognosis by reducing viral replication in mice – Yan – 2018 – Phytotherapy Research – Wiley Online Library. https://onlinelibrary-wiley-com.liboff.ohsu.edu/doi/full/10.1002/ptr.6196. Accessed March 2, 2020.
Shin H-B, Choi M-S, Yi C-M, Lee J, Kim N-J, Inn K-S. Inhibition of respiratory syncytial virus replication and virus-induced p38 kinase activity by berberine. Int Immunopharmacol. 2015;27(1):65-68. doi:10.1016/j.intimp.2015.04.045