 Experts Convene in Autoimmune Summit
Experts Convene in Autoimmune Summit
Wow! I hope all of you got a chance to listen to some of the speakers from this online event which took place Nov. 10-18. Dr. Amy Myers did an excellent job in gathering some of the leading experts, including researchers and clinicians from the fields of immunology, neurology, gastroenterology, and pioneers in the field of functional medicine for this free educational event. Topics ranged from likely causes for this epidemic of autoimmune disease we are now seeing to genetics and environmental triggers of autoimmunity as well as diagnostic testing methods and management of these conditions through dietary and nutrient intervention.
 For those of you that did not have a chance to hear all of these speakers, I have good news: you can still hear any of these talks that you missed! San Jose Functional Medicine has purchased the entire set of presentations and offering direct access of all these talks to our patients, just like we did for the Gluten Summit! Just let us know by email that you are interested in hearing these talks and enter “Autoimmune Summit” in the subject of the email! We will send you a link that you can use to access the entire set of talks so you don’t miss a thing! You can also purchase the entire set of talks directly from the Autoimmune Summit website. Here are some excerpts from the talks of my personal Fab Five speakers from this amazing summit:
For those of you that did not have a chance to hear all of these speakers, I have good news: you can still hear any of these talks that you missed! San Jose Functional Medicine has purchased the entire set of presentations and offering direct access of all these talks to our patients, just like we did for the Gluten Summit! Just let us know by email that you are interested in hearing these talks and enter “Autoimmune Summit” in the subject of the email! We will send you a link that you can use to access the entire set of talks so you don’t miss a thing! You can also purchase the entire set of talks directly from the Autoimmune Summit website. Here are some excerpts from the talks of my personal Fab Five speakers from this amazing summit:
 1. Mark Hyman, MD: A Functional Medicine Approach to Autoimmunity
1. Mark Hyman, MD: A Functional Medicine Approach to Autoimmunity
Dr. Amy Myers: I am thrilled with today’s speaker: we have Dr. Mark Hyman, who is effectively one of my most favorite people on the planet…and really probably does not need an introduction for the listeners out there, but I will give him one as it is. He has eight New York Times bestsellers, his most recent one, The 10-Day Detox Diet. He’s the chairman of the Institute of Functional Medicine. He has a clinic, The Ultra Wellness Center in Lenox, Massachusetts.  He’s been on The Katie Couric Show and now I think is going to be part of The Dr. Oz Show, unless that’s a big secret I hope to not be spoiling…Editor of the Huffington Post, and the list goes on and on… Linus Pauling award winner, really the person who I believe has helped bring functional medicine to the mainstream and really is the pioneer leader of getting the message out. So we appreciate you. You have helped me personally and professionally, so absolutely one of my most favorite people. So I know that you have a personal story, and most of us do in functional medicine of how we got here. So I would love it if you could just share that quickly before we dive into autoimmunity.
He’s been on The Katie Couric Show and now I think is going to be part of The Dr. Oz Show, unless that’s a big secret I hope to not be spoiling…Editor of the Huffington Post, and the list goes on and on… Linus Pauling award winner, really the person who I believe has helped bring functional medicine to the mainstream and really is the pioneer leader of getting the message out. So we appreciate you. You have helped me personally and professionally, so absolutely one of my most favorite people. So I know that you have a personal story, and most of us do in functional medicine of how we got here. So I would love it if you could just share that quickly before we dive into autoimmunity.
 Dr. Mark Hyman: Well actually, in fact, I had a version of an autoimmune disease, an inflammatory condition where I had autoimmune antibodies and my body had broken down. And I had gone from being super healthy—I was a yoga teacher, I was a trainer for 10 years, I ran five miles a day, I’d ride my bike 100 miles a day. And literally, from one day to the next, my body just fell apart, and I developed severe fatigue, cognitive dysfunction, muscle pain—my muscle enzymes went up, my autoimmune antibodies went up, my ANA went up. Liver function tests went up, white count went down, and my digestion went completely upside down. I couldn’t digest food; I had bloating, diarrhea, and gas for years. My whole system just collapsed. Rashes, sores on my tongue, I mean nothing like ever before. I was super healthy. And I was going to have to go on disability, and I could just barely function. And it was through that disease that I discovered functional medicine. And the disease—whatever we call it, it sort of doesn’t matter—but maybe people would say it was chronic fatigue syndrome, it was whatever.
Dr. Mark Hyman: Well actually, in fact, I had a version of an autoimmune disease, an inflammatory condition where I had autoimmune antibodies and my body had broken down. And I had gone from being super healthy—I was a yoga teacher, I was a trainer for 10 years, I ran five miles a day, I’d ride my bike 100 miles a day. And literally, from one day to the next, my body just fell apart, and I developed severe fatigue, cognitive dysfunction, muscle pain—my muscle enzymes went up, my autoimmune antibodies went up, my ANA went up. Liver function tests went up, white count went down, and my digestion went completely upside down. I couldn’t digest food; I had bloating, diarrhea, and gas for years. My whole system just collapsed. Rashes, sores on my tongue, I mean nothing like ever before. I was super healthy. And I was going to have to go on disability, and I could just barely function. And it was through that disease that I discovered functional medicine. And the disease—whatever we call it, it sort of doesn’t matter—but maybe people would say it was chronic fatigue syndrome, it was whatever.
 What happened was that I got a huge load of mercury when I was in China which triggered an immune inflammatory process, destroyed my gut, and led to severe symptoms and muscle damage and mitochondrial injury. And so I had to literally figure out how to fix myself from the ground up, and no one had really mapped this out very well. And I sort of discovered a couple of pioneers in functional medicine: Sidney Baker, Leo Galland, Jeff Bland. I began to learn from them and sit at their feet, go to their clinic, and try and ask for their help, and I slowly started to put myself back together like Humpty Dumpty. And I didn’t really have a good map, and then through the process, I realized functional medicine was evolving, and I became the chairman of the Institute, and we really developed a whole institute of training, certification, and text books. We’re now partnering with the Cleveland Clinic, and we’re doing research in autoimmune disease, so we’re really taking this forward.
What happened was that I got a huge load of mercury when I was in China which triggered an immune inflammatory process, destroyed my gut, and led to severe symptoms and muscle damage and mitochondrial injury. And so I had to literally figure out how to fix myself from the ground up, and no one had really mapped this out very well. And I sort of discovered a couple of pioneers in functional medicine: Sidney Baker, Leo Galland, Jeff Bland. I began to learn from them and sit at their feet, go to their clinic, and try and ask for their help, and I slowly started to put myself back together like Humpty Dumpty. And I didn’t really have a good map, and then through the process, I realized functional medicine was evolving, and I became the chairman of the Institute, and we really developed a whole institute of training, certification, and text books. We’re now partnering with the Cleveland Clinic, and we’re doing research in autoimmune disease, so we’re really taking this forward.
 Through my own journey I figured out how the body works, how it breaks down, what the causes of disease are—not just from a theoretical perspective, but from a cellular perspective. My own body was the living experiment that I used to actually try all this stuff out, and see it work! So many people suffer needlessly, and that’s what drives me. I see people not getting answers to problems that they have. Often autoimmunity is one of the biggest issues people suffer from. It has the worst treatments, and we have the best outcomes, and it just drives me crazy that people don’t know about this.
Through my own journey I figured out how the body works, how it breaks down, what the causes of disease are—not just from a theoretical perspective, but from a cellular perspective. My own body was the living experiment that I used to actually try all this stuff out, and see it work! So many people suffer needlessly, and that’s what drives me. I see people not getting answers to problems that they have. Often autoimmunity is one of the biggest issues people suffer from. It has the worst treatments, and we have the best outcomes, and it just drives me crazy that people don’t know about this.
Dr. Amy Myers: So, in your 15 plus years practicing functional medicine now…have you seen a rise in autoimmunity in your clinic?
Dr. Mark Hyman: Oh yeah. At least, we treat a lot of it. And I think there’s a whole continuum. We often think, you know—and this is kind of weird in medicine, you have this sort of on-and-off diagnosis. You fit these criteria, and you have lupus. You fit these criteria, and you have rheumatoid arthritis. You fit these criteria, you have MS, or whatever, or inflammatory bowel. But we realize now there’s a continuum, and there’s even something called pre-autoimmune disease, which I think is a stupid name, beca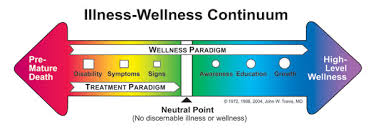 use there’s no “pre” anything. It’s all a continuum of imbalances that go from mild, to moderate, to severe, to deadly. So I think that my role is to really look at that whole spectrum.
use there’s no “pre” anything. It’s all a continuum of imbalances that go from mild, to moderate, to severe, to deadly. So I think that my role is to really look at that whole spectrum.
You’re looking at the whole spectrum and it’s dramatically on the rise, in fact. There are about 9 million people with cancer, 22 million people with heart disease. There are 24 million people with autoimmune disease, and it’s on the rise. So when you take it as a collective problem and you look at them together, there are 80 autoimmune diseases. It’s a huge issue. Whether it’s arthritis, lupus, inflammatory bowel, MS, Sjögren’s, or vitiligo, or all sorts of autoimmune things… psoriasis…it’s such a huge problem that people haven’t seen it as one problem. And there’s no sort of autoimmune society, there’s no autoimmune institute. There’s like all these different pieces that are treated and looked at by different people, and nobody’s looking at the problem as one whole continuing issue.
Dr. Amy Myers: So, based on the statistics you were just giving—and I’ve heard it’s the third leading chronic disease—but based on the statistics you just gave, it sounds like it’s actually the leading chronic disease.
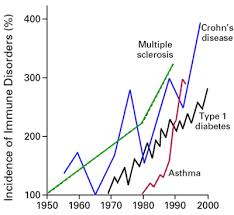 Dr. Mark Hyman: Well, yeah. It really is. I think when we look at the number of people affected by it, yes. I mean, it’s huge. I mean, diabetes is up there, it’s like 27 million. But it’s in there. It’s in the range. It’s such a heterogeneous group of diseases, right? It affects 8% of our population—the problem is that less than a third are diagnosed. So we’ve got 17 million people maybe who actually have it. And it affects hundreds of millions worldwide, rates are increasing dramatically. There’s a latent period of 7-14 years where it’s not even diagnosed and it’s sort of “pre-autoimmunity.” And often it’s only diagnosed after there’s tissue destruction instead of when there are imbalances that can be picked up early. So I really think it’s important to identify the trends in people’s bodies and see… I screen for that routinely. It’s really the third leading cause of morbidity and mortality after heart disease and cancer. Heart disease and cancer kill people and make people really sick, but autoimmune disease is right up there. And the healthcare costs are twice that of cancer.
Dr. Mark Hyman: Well, yeah. It really is. I think when we look at the number of people affected by it, yes. I mean, it’s huge. I mean, diabetes is up there, it’s like 27 million. But it’s in there. It’s in the range. It’s such a heterogeneous group of diseases, right? It affects 8% of our population—the problem is that less than a third are diagnosed. So we’ve got 17 million people maybe who actually have it. And it affects hundreds of millions worldwide, rates are increasing dramatically. There’s a latent period of 7-14 years where it’s not even diagnosed and it’s sort of “pre-autoimmunity.” And often it’s only diagnosed after there’s tissue destruction instead of when there are imbalances that can be picked up early. So I really think it’s important to identify the trends in people’s bodies and see… I screen for that routinely. It’s really the third leading cause of morbidity and mortality after heart disease and cancer. Heart disease and cancer kill people and make people really sick, but autoimmune disease is right up there. And the healthcare costs are twice that of cancer.
Dr. Amy Myers: Yeah. And so why is that? Why is it not getting diagnosed? Why is it so fractured? Why are the healthcare costs so expensive?
 Dr. Mark Hyman: Well it’s not getting diagnosed because most doctors are not aggressively looking for it, and they often wait until the symptoms are dramatic or extreme. So we don’t diagnose it, and I think that’s a problem. We have to get smarter about diagnosing it and seeing how to identify the root causes.
Dr. Mark Hyman: Well it’s not getting diagnosed because most doctors are not aggressively looking for it, and they often wait until the symptoms are dramatic or extreme. So we don’t diagnose it, and I think that’s a problem. We have to get smarter about diagnosing it and seeing how to identify the root causes.
Dr. Amy Myers: Do you think part of that is also because they don’t really have effective treatments? I mean, a lot of people say with underactive thyroid that the doctor doesn’t really care if it’s Hashimoto’s or not, because they’re not going to treat it differently. Whereas you and I…that puts someone in a completely different category for us.
Dr. Mark Hyman: Right. I mean, here’s the thing. What is autoimmune disease? It’s an inflammatory disease. And the question then becomes not “How do I shut off inflammation?” but “How do I find the root cause of inflammation? Why is  the immune system so pissed off?” That’s a question that most doctors don’t ask, so what we do in conventional care is we block, antagonize, suppress, and inhibit the immune system. We use anti-inflammatory drugs like nonsteroidals, whether it’s Aleve or Advil. We use steroids, we use drugs called TNF-alpha blockers which are called “disease modifying drugs” that suppress immunity and cause cancer, or an overwhelming infection. We’ll use chemo drugs—methotrexate, Imuran, cyclosporine—we’ve been using bone marrow transplants for some people. These are extremely aggressive, extremely intense drugs with tons of side effects. I mean, listen, if you could take a pill like a vitamin or like a mild drug that didn’t really have all these side effects and it cured autoimmune disease, great! But we don’t have that. So the problem is that there are a lot of approaches that are being missed, and doctors don’t really think there is a cure.
the immune system so pissed off?” That’s a question that most doctors don’t ask, so what we do in conventional care is we block, antagonize, suppress, and inhibit the immune system. We use anti-inflammatory drugs like nonsteroidals, whether it’s Aleve or Advil. We use steroids, we use drugs called TNF-alpha blockers which are called “disease modifying drugs” that suppress immunity and cause cancer, or an overwhelming infection. We’ll use chemo drugs—methotrexate, Imuran, cyclosporine—we’ve been using bone marrow transplants for some people. These are extremely aggressive, extremely intense drugs with tons of side effects. I mean, listen, if you could take a pill like a vitamin or like a mild drug that didn’t really have all these side effects and it cured autoimmune disease, great! But we don’t have that. So the problem is that there are a lot of approaches that are being missed, and doctors don’t really think there is a cure.
 In fact, I just saw a patient yesterday who I’ve been seeing for almost a decade. And when she came to see me, she had severe rheumatoid arthritis, her auto-antibodies were like—her ANA was 1 to 1280, which is a very high number– she had severe joint pains and rheumatoid arthritis, she had migraines, she had irritable bowel syndrome, she had terrible fatigue, and she was really quite sick. She had sinus issues and all sorts of issues, right? And this is common for these people, but they just treat everything separately, so they see a neurologist for the migraine, a G.I. guy for the irritable bowel, the rheumatologist for the autoimmune disease, and they’re really all connected. So we found out she in fact had very high anti-gliadin antibodies in her blood, which is a sign of gluten sensitivity. She didn’t have true celiac, but close. And she had super high levels of mercury like 120, and she also had immune response to mercury.
In fact, I just saw a patient yesterday who I’ve been seeing for almost a decade. And when she came to see me, she had severe rheumatoid arthritis, her auto-antibodies were like—her ANA was 1 to 1280, which is a very high number– she had severe joint pains and rheumatoid arthritis, she had migraines, she had irritable bowel syndrome, she had terrible fatigue, and she was really quite sick. She had sinus issues and all sorts of issues, right? And this is common for these people, but they just treat everything separately, so they see a neurologist for the migraine, a G.I. guy for the irritable bowel, the rheumatologist for the autoimmune disease, and they’re really all connected. So we found out she in fact had very high anti-gliadin antibodies in her blood, which is a sign of gluten sensitivity. She didn’t have true celiac, but close. And she had super high levels of mercury like 120, and she also had immune response to mercury.
 So we looked at the causes, and we said, “Gee, it’s mercury and gluten, leaky gut…” she had tremendous overgrowth of yeast in her gut, so we had to kind of fix her gut. We had to get rid of the gluten, we had to get rid of the mercury, and over time, she has completely normalized. She’s 65 now, and she’s as healthy as she’s ever been. She has no auto-antibodies—she went from 1,280 to 0. Her gluten antibodies went down completely to normal. Her mercury went from 120 to 5, and her symptoms are completely better. She’s had no migraines in years and years and no irritable bowel. She’s full of energy and has no autoimmunity at all! So most doctors don’t even think that that’s possible, and they don’t even bother checking the autoantibodies if they’ve been diagnosed initially, because they figure they’re just never going to go down. But they do go away if you do the right thing, if you get to the cause.
So we looked at the causes, and we said, “Gee, it’s mercury and gluten, leaky gut…” she had tremendous overgrowth of yeast in her gut, so we had to kind of fix her gut. We had to get rid of the gluten, we had to get rid of the mercury, and over time, she has completely normalized. She’s 65 now, and she’s as healthy as she’s ever been. She has no auto-antibodies—she went from 1,280 to 0. Her gluten antibodies went down completely to normal. Her mercury went from 120 to 5, and her symptoms are completely better. She’s had no migraines in years and years and no irritable bowel. She’s full of energy and has no autoimmunity at all! So most doctors don’t even think that that’s possible, and they don’t even bother checking the autoantibodies if they’ve been diagnosed initially, because they figure they’re just never going to go down. But they do go away if you do the right thing, if you get to the cause.
Dr. Amy Myers: So what are you seeing in your clinic as the top causes for autoimmunity?
Dr. Mark Hyman: I think, Amy, it’s really important to think about the framework of functional medicine. So that’s a method we have for figuring out what the causes are. And it’s really a simple process. We say, “What is it that could be bugging you that’s triggering inflammation?” And we need to get rid of that. “What is it that you need for your immune system to work  properly, for your body to work properly?” And we try to give you those things. So we get rid of the bad stuff, and we put in the good stuff. The bad stuff is a short list, and I think it’s really important to understand what those causes are, and they’re different for different people, so you can have 10 people with exactly the same autoimmune disease, and each one of those 10 people might have a different set of causes. So you can’t treat them all the same, right? And that’s really important. One person might have an autoimmune disease from eating gluten, and another person might be from mercury, and another person might be from a parasite in their gut, and the list goes on and on. Other people with strongyloides, which is a weird worm that people get, causes autoimmunity. But like, who knew that? You have to treat that person with a worm pill, another person you have to do chelation, and for another person you have to change their diet. Very different treatments for the exact same disease. And that’s the beauty of functional medicine—it allows you to figure that out.
properly, for your body to work properly?” And we try to give you those things. So we get rid of the bad stuff, and we put in the good stuff. The bad stuff is a short list, and I think it’s really important to understand what those causes are, and they’re different for different people, so you can have 10 people with exactly the same autoimmune disease, and each one of those 10 people might have a different set of causes. So you can’t treat them all the same, right? And that’s really important. One person might have an autoimmune disease from eating gluten, and another person might be from mercury, and another person might be from a parasite in their gut, and the list goes on and on. Other people with strongyloides, which is a weird worm that people get, causes autoimmunity. But like, who knew that? You have to treat that person with a worm pill, another person you have to do chelation, and for another person you have to change their diet. Very different treatments for the exact same disease. And that’s the beauty of functional medicine—it allows you to figure that out.
 And I think the things we really think about are, “What are the toxins?” Like this woman I mentioned, she had high levels of mercury, there was this immunotoxin that caused inflammation. We measured how her cells—her lymphocytes—were responding to mercury, and we saw that they were really upset that the mercury was around. They were creating a trigger. But there are also other toxins, all the chemicals and pesticides, the plastics we’re exposed to—they’re what we call autogens. There are triggers that are chemicals that cause an autoimmune response. They’re called autogens. They’re also called obesogens because they cause obesity, too. They do everything.
And I think the things we really think about are, “What are the toxins?” Like this woman I mentioned, she had high levels of mercury, there was this immunotoxin that caused inflammation. We measured how her cells—her lymphocytes—were responding to mercury, and we saw that they were really upset that the mercury was around. They were creating a trigger. But there are also other toxins, all the chemicals and pesticides, the plastics we’re exposed to—they’re what we call autogens. There are triggers that are chemicals that cause an autoimmune response. They’re called autogens. They’re also called obesogens because they cause obesity, too. They do everything.
And then there are allergens we’re exposed to. They can be things we’re eating, and that’s the biggest source. Gluten, dairy, grains, are often a big trigger. Mold, environmental allergens, even chemical allergens can trigger a problem. Microbes, bugs—not just bugs in your gut, abnormal gut flora, which we have like parasites, yeast, bad bugs—but also things like tick-borne diseases and other weird viruses and chronic viral infections. These are things that your immune system starts reacting to. So there’s a process called molecular mimicry where our bodies start to react to these various triggers that are infectious. And then of course there’s stress. Both physical and psychological stress will trigger inflammation and autoimmunity. And poor diet. When you eat a bad diet, you’re actually affecting your gut flora. You’re creating inflammation just from the sugar. So there are a lot of things in your diet that can actually change the equation and push you toward autoimmunity.
 2. David Perlmutter, MD: The Brain, Gut, and Autoimmunity
2. David Perlmutter, MD: The Brain, Gut, and Autoimmunity
Dr. Amy Myers: Today, we have Dr. David Perlmutter with us. I’m sure many of you know who he is. He’s the author of “Grain Brain,” which I know has really kind of catapulted him into mainstream, which is awesome, and also the author of “The Grain Brain Cookbook” that I think will be out in two weeks? And Grain Brain is now on its 17th publishing and is in 28 countries, and has been on the New York best seller list for 44 weeks.  Besides all that, he also actually has a very active practice in Florida. And you’re on the faculty of Institute of Functional Medicine and you are a board-certified neurologist. I think I heard you in another interview and somebody said, “We all know we refer to the gut as the second brain,” and you said that it actually may be the first brain.
Besides all that, he also actually has a very active practice in Florida. And you’re on the faculty of Institute of Functional Medicine and you are a board-certified neurologist. I think I heard you in another interview and somebody said, “We all know we refer to the gut as the second brain,” and you said that it actually may be the first brain.
Dr. David Perlmutter: Might well be. If you think of what’s going on in the gut in terms of its genetic potential, in terms of what the gut bacteria can do in terms of human metabolism, obesity, inflammation, autoimmunity, that’s where it starts. Those are the key players in brain degenerative conditions like Parkinson’s and multiple sclerosis, Alzheimer’s, and even things like autism, and to some degree, even ADHD so prevalent in Western cultures, and we’re now really getting a handle on  the notion that the gut has a huge influence on what goes on in the brain. And I’m sure that you and I will talk about that.
the notion that the gut has a huge influence on what goes on in the brain. And I’m sure that you and I will talk about that.
Dr. Amy Myers: Absolutely. Well, let’s first get into kind of what is brain inflammation?
Dr. David Perlmutter: Well, it’s nothing different than anyone else is familiar with. It’s the same process of creating life-sustaining inflammatory chemicals—there’s a good side to inflammation. It helps us deal with infection, it helps us immobilize a damaged part, but the downside is when it’s chronic, it increases free radicals, it damages our DNA, our fat, our protein, and leads to tissue destruction. It’s why the arthritic joint becomes destroyed; it’s why the inflamed coronary arteries become narrow; and it’s the same causes that underlies why a person’s brain will shrink when he or she is becoming demented. So, in the brain, we don’t re ally appreciate inflammation as readily because when your brain is inflamed, it doesn’t hurt, it doesn’t become red, it doesn’t get swollen.
ally appreciate inflammation as readily because when your brain is inflamed, it doesn’t hurt, it doesn’t become red, it doesn’t get swollen.
We don’t really get the opportunity to appreciate the simple fact that inflammation underlies things like Alzheimer’s now affecting 5.4 million Americans and inflammatory disorders really for the most part, not a genetic disorder, not a genetic inheritance issue, but perhaps some genetic predisposition, but more importantly, absolutely, fundamentally related to our lifestyle choices that increase inflammation, and these are centered upon, for example, the very foods that we eat, leading to inflammation throughout the body, and clearly, being related to developing an incurable disease, at least, as you and I have this conversation, called “Alzheimer’s,” related to the foods that we eat. That’s an important conversation to have.
Dr. Amy Myers: And what really is that role? So, inflammation is, you’re saying, is leading to these diseases. How is it really doing that?
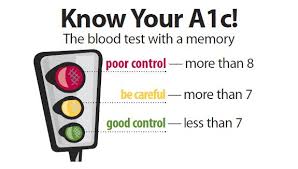 Dr. David Perlmutter: Well, I guess what you’re asking is the mechanism. Until recently, I think a lot of interest has been focused on what is called “glycation of proteins,” meaning that the higher your blood sugar is, the more your blood sugar will bind to proteins in a process called glycation. We measure that, for example, with the playing old-fashioned HbA1c test –the diabetics use to measure their average blood sugar. Well, it turns out that as a metric, HbA1c—a measurement of your average blood sugar (let’s just say “glycated protein”)—powerfully relates to the rate at which your brain shrinks. Higher A1c, even well below the levels that are qualified for diagnosing diabetes, directly correlate with the rate at which your brain shrinks, so that’s something you don’t want to have.
Dr. David Perlmutter: Well, I guess what you’re asking is the mechanism. Until recently, I think a lot of interest has been focused on what is called “glycation of proteins,” meaning that the higher your blood sugar is, the more your blood sugar will bind to proteins in a process called glycation. We measure that, for example, with the playing old-fashioned HbA1c test –the diabetics use to measure their average blood sugar. Well, it turns out that as a metric, HbA1c—a measurement of your average blood sugar (let’s just say “glycated protein”)—powerfully relates to the rate at which your brain shrinks. Higher A1c, even well below the levels that are qualified for diagnosing diabetes, directly correlate with the rate at which your brain shrinks, so that’s something you don’t want to have.
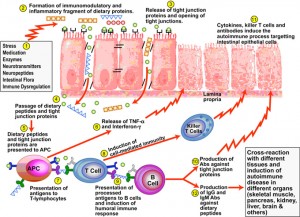
 That said, the mechanism is that when proteins become glycated, it turns on genetic pathways that amp up the production of these inflammatory chemicals called “cytokines.” Now, beyond that, a newer mechanism that is becoming really quite exciting for those of us who are looking beyond the brain, has to do with the role of these glycated proteins—again, brought on by having high blood sugar—in terms of their increased permeability events in terms of the gut. In other words, glycated proteins, these things called “AGEs (advanced glycosylated end-products)” or AGEs, protein bound to sugar, increases the leakiness of the gut. When the gut is leaky, that is just like turning on gasoline to the flames of inflammation. When the gut becomes leaky—to be technical about it—what happens is there is a coating over what are called “gram-negative bacteria,” which are hugely represented in the gut. When that coating, that goes by the initials “LPS” makes its way to the systemic circulation, it just causes inflammation to go haywire. Elevated levels of this LPS, which correlate to dramatic increased inflammation, are strongly correlated with Alzheimer’s, even Lou Gehrig’s disease for that matter.
That said, the mechanism is that when proteins become glycated, it turns on genetic pathways that amp up the production of these inflammatory chemicals called “cytokines.” Now, beyond that, a newer mechanism that is becoming really quite exciting for those of us who are looking beyond the brain, has to do with the role of these glycated proteins—again, brought on by having high blood sugar—in terms of their increased permeability events in terms of the gut. In other words, glycated proteins, these things called “AGEs (advanced glycosylated end-products)” or AGEs, protein bound to sugar, increases the leakiness of the gut. When the gut is leaky, that is just like turning on gasoline to the flames of inflammation. When the gut becomes leaky—to be technical about it—what happens is there is a coating over what are called “gram-negative bacteria,” which are hugely represented in the gut. When that coating, that goes by the initials “LPS” makes its way to the systemic circulation, it just causes inflammation to go haywire. Elevated levels of this LPS, which correlate to dramatic increased inflammation, are strongly correlated with Alzheimer’s, even Lou Gehrig’s disease for that matter.
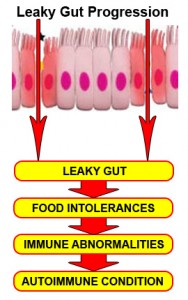 Depression, for example, is now looked upon as a smoldering inflammatory event in the human brain brought on by leakiness of the gut. So, how incredible it is, Dr. Myers that you and I are having a conversation about things that go on in the brain and we are exploring the health of the gut as it relates to the brain. So, it’s all about maintenance of the integrity of the gut lining, whether we’re talking about coronary artery disease, lupus, diabetes type 1, any autoimmune phenomenon, or any inflammatory condition in human physiology, we’ve got to pay very strict attention to all of the factors that play a role in maintaining the gut wall integrity. And understand that this lining of the gut that is the focus of so much research that really mediates whether things get in or not is one cell thick. Can you imagine? One cell thick with the surface area of a tennis court—not the one the cell, but the whole gut lining. This mediates what gets in and what gets out.
Depression, for example, is now looked upon as a smoldering inflammatory event in the human brain brought on by leakiness of the gut. So, how incredible it is, Dr. Myers that you and I are having a conversation about things that go on in the brain and we are exploring the health of the gut as it relates to the brain. So, it’s all about maintenance of the integrity of the gut lining, whether we’re talking about coronary artery disease, lupus, diabetes type 1, any autoimmune phenomenon, or any inflammatory condition in human physiology, we’ve got to pay very strict attention to all of the factors that play a role in maintaining the gut wall integrity. And understand that this lining of the gut that is the focus of so much research that really mediates whether things get in or not is one cell thick. Can you imagine? One cell thick with the surface area of a tennis court—not the one the cell, but the whole gut lining. This mediates what gets in and what gets out.
There are obviously pathways that selectively allow things to get in that we need, but when those junctions have been traumatized by, in this case, glycation of proteins from having too high of a blood sugar, then things like proteins, and as I mentioned before, LPS (which is the covering of the gram-negative bacteria) get in to the systemic circulation and just beef up inflammation, and that basically sets the stage for things going on fire. And unfortunately, our efforts to take care of these diseases don’t focus on the fire of inflammation. We basically tend, in modern medicine, to focus only on the smoke. So, if you’re suffering from an inflammatory condition, you’re given an anti-inflammatory medication like, for example, a non-steroidal anti-inflammatory medicine, which are used by millions of Americans to treat inflammatory disorders like arthritis, and what these drugs do in the long run is they further damage the gut lining making the fire worse while people, moment to moment, feel a little bit better, but the problem worsens.
 So, we’ve got to really start pay strict attention if we’re going to have leverage points in neurological conditions like ADHD and autism, Parkinson’s, multiple sclerosis, and Alzheimer’s. We’ve got to pay attention to what is going on in the gut, and that means we’ve got to pay attention to the overusage of antibiotics that damage the gut bacteria. The explosive overusage of antibiotics in cattle that are then consumed by us—that’s where 70-80% of the antibiotics in America are used. We’ve got to understand that the very medication we are using to treat inflammation are damaging the gut lining, and we’ve even got to take this back to how you were born. The method of fetal delivery is how we inoculate the gut bacteria from the get-go—that when that child passes through the mother’s birth canal, the bacteria are invested into the mouth to begin populating the gut and that sets the stage for inflammation for that child for the rest of his or her lifetime. That either sets the stage for an autoimmune condition like type-1 diabetes or celiac disease, or it sets the stage for that immune system to be perfectly balanced and adaptable and able to confront changes in the environment as that individual grows up.
So, we’ve got to really start pay strict attention if we’re going to have leverage points in neurological conditions like ADHD and autism, Parkinson’s, multiple sclerosis, and Alzheimer’s. We’ve got to pay attention to what is going on in the gut, and that means we’ve got to pay attention to the overusage of antibiotics that damage the gut bacteria. The explosive overusage of antibiotics in cattle that are then consumed by us—that’s where 70-80% of the antibiotics in America are used. We’ve got to understand that the very medication we are using to treat inflammation are damaging the gut lining, and we’ve even got to take this back to how you were born. The method of fetal delivery is how we inoculate the gut bacteria from the get-go—that when that child passes through the mother’s birth canal, the bacteria are invested into the mouth to begin populating the gut and that sets the stage for inflammation for that child for the rest of his or her lifetime. That either sets the stage for an autoimmune condition like type-1 diabetes or celiac disease, or it sets the stage for that immune system to be perfectly balanced and adaptable and able to confront changes in the environment as that individual grows up.
 Dr. Amy Myers: I don’t know if you’ve ever seen that movie, “The Business of Being Born,” but anybody watching this if they haven’t and they’re anticipating getting pregnant or are pregnant, I highly recommend it. It’s talking about the rise of C-sections in the United States now, and even if you’re not wanting it for just convenience, just how it got into somehow being in labor for 10 hours or 12 hours became unacceptable, and that was too long, or your baby wasn’t delivered right at 40 weeks and you’ve gone to 41 or 42 and suddenly, they have to induce and then when they do, giving that Pitocin then stimulates contractions, get the baby in distress and then it’s creating the C-section.
Dr. Amy Myers: I don’t know if you’ve ever seen that movie, “The Business of Being Born,” but anybody watching this if they haven’t and they’re anticipating getting pregnant or are pregnant, I highly recommend it. It’s talking about the rise of C-sections in the United States now, and even if you’re not wanting it for just convenience, just how it got into somehow being in labor for 10 hours or 12 hours became unacceptable, and that was too long, or your baby wasn’t delivered right at 40 weeks and you’ve gone to 41 or 42 and suddenly, they have to induce and then when they do, giving that Pitocin then stimulates contractions, get the baby in distress and then it’s creating the C-section.
Dr. David Perlmutter: In America, about 33-34% of births right now are via C-section. In other countries, it may be as high as even—in one city in Rome, 80% of births are via C-section. You’ve got to understand that the process of being born, passing through the birth canal is probably one of the most fundamental events in developing a person’s immune system. That lifelong consequences of being born by cesarean section are, in fact, very real. The risk, for example, of becoming autistic doubles if an individual is born via cesarean section. The risk, for example, of developing an autoimmune celiac disease is increased by about 80%. So, these are real issues. Type-1 diabetes risk is 70% increased. ADHD risk is tripled. The risk of having a child with ADHD is tripled if that child doesn’t pass through the birth canal and becomes inoculated with mother’s vaginal bacteria.
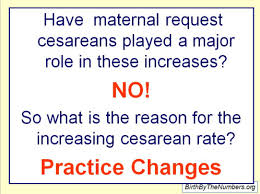 Now, maybe this is a discussion that people might be uncomfortable with, but we’ve got to get over that because this is marking that child for the rest of his or her life. These are real statistics from peer-reviewed medical literature that are really raising a red flag. These are the types of numbers that women need to understand before they get penciled in for a C-section next Thursday at noon. Clearly, cesareans are lifesaving for a mother and a baby—no question there’s a need for that—but that might occur in up to 10% of births, and the fact that there are 33% or 1/3 of all births in America happening via C-section, I think it’s because women and their husbands need to become better informed. As that happens, these statistics will improve.
Now, maybe this is a discussion that people might be uncomfortable with, but we’ve got to get over that because this is marking that child for the rest of his or her life. These are real statistics from peer-reviewed medical literature that are really raising a red flag. These are the types of numbers that women need to understand before they get penciled in for a C-section next Thursday at noon. Clearly, cesareans are lifesaving for a mother and a baby—no question there’s a need for that—but that might occur in up to 10% of births, and the fact that there are 33% or 1/3 of all births in America happening via C-section, I think it’s because women and their husbands need to become better informed. As that happens, these statistics will improve.
 Now, there is also research that indicates that you don’t undo the damage to the microbiome or the gut bacteria by breastfeeding. While breastfeeding is also clearly critically important in the development of the gut bacteria, it doesn’t fully offset those changes that are imparted by a cesarean section. And even to take it further, the mother’s prenatal diet changes the bacteria in the birth canal, whether she is overweight or not has a dramatic effect on the bacteria in the birth canal, and therefore, that is passed on to the newborn baby. That said, we know that women who are overweight give birth to babies who have a higher tendency to become obese. These babies inherit, if you will—it’s not Mendelian inheritance, it’s not sperm-and-egg, gene-DNA inheritance—but they inherit the microbiome of mother that does tend to coat for weight gain, gives them bacteria that tend to be more thrifty, that hold on to calories, and that’s a heck of a thing to saddle a kid with. Rewriting his or her destiny towards obesity just because of the changes that have happened to his or her gut bacteria—the microbiome.
Now, there is also research that indicates that you don’t undo the damage to the microbiome or the gut bacteria by breastfeeding. While breastfeeding is also clearly critically important in the development of the gut bacteria, it doesn’t fully offset those changes that are imparted by a cesarean section. And even to take it further, the mother’s prenatal diet changes the bacteria in the birth canal, whether she is overweight or not has a dramatic effect on the bacteria in the birth canal, and therefore, that is passed on to the newborn baby. That said, we know that women who are overweight give birth to babies who have a higher tendency to become obese. These babies inherit, if you will—it’s not Mendelian inheritance, it’s not sperm-and-egg, gene-DNA inheritance—but they inherit the microbiome of mother that does tend to coat for weight gain, gives them bacteria that tend to be more thrifty, that hold on to calories, and that’s a heck of a thing to saddle a kid with. Rewriting his or her destiny towards obesity just because of the changes that have happened to his or her gut bacteria—the microbiome.
 I think, more information remains (to be discovered) with the topic of this summit that is autoimmunity, and to be super clear, autoimmunity is a delicate balance between a malfunctioning immune system that’s either too active or one that is underactive, in which case we’re susceptible to all kinds of infection. Overactivity of the immune system to the extent that the body fails to differentiate between self and non-self—the cornerstone of autoimmunity—is really set by what goes on the gut bacteria. So, these factors of early life exposure to antibiotics for every sniffle or sore ear that a child might have, the continued push for women to use formula when they’re given samples right when they get out of the delivery room before they leave the hospital, the continued overusage of antibiotics in the production of food, meat, and even as mentioned, this overusage of cesarean section is setting up a generation of newborns for conditions that are life-threatening and in my business, for conditions that threaten brain health, and it’s preventable by getting this information to the population in general.
I think, more information remains (to be discovered) with the topic of this summit that is autoimmunity, and to be super clear, autoimmunity is a delicate balance between a malfunctioning immune system that’s either too active or one that is underactive, in which case we’re susceptible to all kinds of infection. Overactivity of the immune system to the extent that the body fails to differentiate between self and non-self—the cornerstone of autoimmunity—is really set by what goes on the gut bacteria. So, these factors of early life exposure to antibiotics for every sniffle or sore ear that a child might have, the continued push for women to use formula when they’re given samples right when they get out of the delivery room before they leave the hospital, the continued overusage of antibiotics in the production of food, meat, and even as mentioned, this overusage of cesarean section is setting up a generation of newborns for conditions that are life-threatening and in my business, for conditions that threaten brain health, and it’s preventable by getting this information to the population in general.
 3. Alessio Fasano, MD: The Role of Gut Permeability in Autoimmune Diseases: How to Distinguish Facts From Fantasies
3. Alessio Fasano, MD: The Role of Gut Permeability in Autoimmune Diseases: How to Distinguish Facts From Fantasies
Dr. Amy Myers: I could not be more pleased about our guest today. This is really one of the top interviews I’ve been waiting for this entire summit. You’ve heard his name come up left and right in pretty much everybody’s talk about gluten and leaky gut. We have Dr. Alessio Fasano here, who is a world-renowned pediatric gastroenterologist. He is the man who really has done the research behind leaky gut, zonulin, autoimmunity, celiac, and he has founded the Center for Celiac Research, which is now at Massachusetts General Hospital.  He’s also a visiting professor at Harvard, and recently, wrote a book called “Gluten Freedom,” which I have been reading. So, you wrote in a very, sort of groundbreaking article that was the cover of Scientific American…I don’t know if that was five years or six years ago, but you kind of talked about this stool and having three legs of a stool in order to get celiac disease and then we can extrapolate that out to all autoimmune diseases about sort of genetics, the environment, and the gut. Can you speak to that?
He’s also a visiting professor at Harvard, and recently, wrote a book called “Gluten Freedom,” which I have been reading. So, you wrote in a very, sort of groundbreaking article that was the cover of Scientific American…I don’t know if that was five years or six years ago, but you kind of talked about this stool and having three legs of a stool in order to get celiac disease and then we can extrapolate that out to all autoimmune diseases about sort of genetics, the environment, and the gut. Can you speak to that?
Dr. Alessio Fasano: Sure. You know, you also have to appreciate that this has been very challenging to put this concept forward so we were really kind of current, and it was an uphill battle, starting with the concept to convince the colleagues in the scientific community in general that celiac disease is an autoimmune disease. Again, there was very reluctant acceptance to the concept because the paradigm was, in autoimmunity, it’s something you cannot treat. It’s a one-way direction; when you got it, that’s it. With celiac disease being treatable with the diet—people, they really had a hard time to grasp the concept that this indeed was an autoimmune disease. Now, nobody would dispute that. But because this was a one of a kind autoimmune disease, we were able to really study in great detail what are the tools, what are the ingredients of this recipe, if you wish, and that’s how we learned that indeed, there are three pillars that you need to have in order to develop autoimmunity.
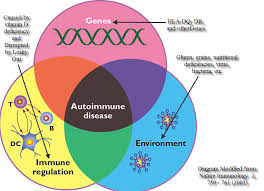 One is you have to be genetically predisposed, and nobody would dispute that. You have to have many genes involved. With great frustration, we’ve focused lot of attention to find “the genes of autoimmunity,” just to find ourselves with empty hands because the more you search, the more genes come out. The Human Genome Project taught us that that’s definitely not the way to go to learn what is the genetic composition of autoimmunity because there’s a lot of variability, and so on and so forth, but definitely, there are many genes that you need to have in order to develop an autoimmune disease.
One is you have to be genetically predisposed, and nobody would dispute that. You have to have many genes involved. With great frustration, we’ve focused lot of attention to find “the genes of autoimmunity,” just to find ourselves with empty hands because the more you search, the more genes come out. The Human Genome Project taught us that that’s definitely not the way to go to learn what is the genetic composition of autoimmunity because there’s a lot of variability, and so on and so forth, but definitely, there are many genes that you need to have in order to develop an autoimmune disease.
The second component is an environmental trigger, something that is mismanaged by the immune system because of its genetic makeup. The immune system, in general, is all there to defend us against these enemies that can harm our body, but in people with genetic disposition to autoimmunity, the weapons of the immune system, rather to be directed against the enemy, is directed against your own body. A different target organ can develop into a different disease, such as diabetes, MS (multiple sclerosis), or celiac disease. Celiac disease is unique, because we know the enemy that we don’t know for any other autoimmune disease (that is gluten), and therefore we know that if there’s any way to stop this interplay between the genes and the environment, in this case, by eliminating one of the two ingredients, you can stop autoimmunity.
 We start really to get more insights of what it takes to develop autoimmunity and that would allow us to learn the third pillar—loss of barrier function by the intestine—that becomes more permeable and therefore allows these enemies to more easily gain access in our body and therefore to be exposed to the immune system that can react in an inappropriate way. So again, this concept—others say unforeseen, not really generally accepted, or fully-formed thinking of concepts—was put out there, and the Scientific American article that was published roughly five years ago was indeed, the stone in the pond, and the waves started to move, and nevertheless there was mixed feeling in terms of accepting this concept mainly because this increased permeability, this leaky gut syndrome had been vilified according to the scientific establishment. Complementary alternative medicine seems to claim that everything that goes wrong is due to the leaky gut, and people have a hard time believing that, and therefore, people had a really hard time to accept the concept. But now, I think that the evidence, not only from our group, but from many other people that studied it, is pretty overwhelmingly clear that there you need all three elements to develop autoimmunity.
We start really to get more insights of what it takes to develop autoimmunity and that would allow us to learn the third pillar—loss of barrier function by the intestine—that becomes more permeable and therefore allows these enemies to more easily gain access in our body and therefore to be exposed to the immune system that can react in an inappropriate way. So again, this concept—others say unforeseen, not really generally accepted, or fully-formed thinking of concepts—was put out there, and the Scientific American article that was published roughly five years ago was indeed, the stone in the pond, and the waves started to move, and nevertheless there was mixed feeling in terms of accepting this concept mainly because this increased permeability, this leaky gut syndrome had been vilified according to the scientific establishment. Complementary alternative medicine seems to claim that everything that goes wrong is due to the leaky gut, and people have a hard time believing that, and therefore, people had a really hard time to accept the concept. But now, I think that the evidence, not only from our group, but from many other people that studied it, is pretty overwhelmingly clear that there you need all three elements to develop autoimmunity.
 Dr. Amy Myers: And so, do you feel that gluten is a problem for all autoimmune diseases or only for celiac disease?
Dr. Amy Myers: And so, do you feel that gluten is a problem for all autoimmune diseases or only for celiac disease?
Dr. Alessio Fasano: Oh no, I don’t think that gluten is the culprit for all autoimmune diseases at all. And matter of fact, while we have an undisputable law for celiac disease and we know because factually we take gluten out of the diet and people with celiac disease will have symptoms resolved, will have the alpha antibodies gone and will have the autoimmune insult that was first defined by the damage, repaired. We don’t have that strong evidence with anything else. We have some hints that gluten may have a role in type-1 diabetes, may have a role in multiple sclerosis, maybe that is a tangential and not the principal role like in celiac disease, but definitely, we don’t have the undisputable evidence that it can be really responsible for all of this.
Dr. Amy Myers: But leaky gut, you would say, is something that does need to be present in other autoimmune diseases or not necessarily as well?
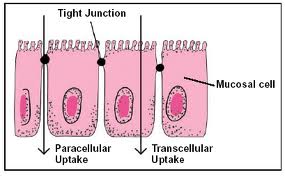
 Dr. Alessio Fasano: I think that that’s a must. I’m very biased here because I’m not an expert immunologist, so again, I trust and respect deeply the opinion of my colleague immunologists. I am an expert in gut physiology and biology, and if you accept, and everybody does, that the main port of entry of this instigator of autoimmunity is the gut…if you don’t have a loss of this barrier function, I just can’t see how molecules—that need to be large, these proteins, that are instigating the immune response—can get access and be seen by the immune system, because under normal circumstances, the gut has this formidable capability to keep at bay large molecules, potential enemies outside our body. Therefore, I don’t see how you can instigate an immune response unless physically, the immune system that is within our body and these enemies that are outside are body, see each other, touch each other, and are physically interacting. And again, the reason why, for example, there are a lot of medications that we cannot give by mouth is because they are too large, we have to give by injection like insulin.
Dr. Alessio Fasano: I think that that’s a must. I’m very biased here because I’m not an expert immunologist, so again, I trust and respect deeply the opinion of my colleague immunologists. I am an expert in gut physiology and biology, and if you accept, and everybody does, that the main port of entry of this instigator of autoimmunity is the gut…if you don’t have a loss of this barrier function, I just can’t see how molecules—that need to be large, these proteins, that are instigating the immune response—can get access and be seen by the immune system, because under normal circumstances, the gut has this formidable capability to keep at bay large molecules, potential enemies outside our body. Therefore, I don’t see how you can instigate an immune response unless physically, the immune system that is within our body and these enemies that are outside are body, see each other, touch each other, and are physically interacting. And again, the reason why, for example, there are a lot of medications that we cannot give by mouth is because they are too large, we have to give by injection like insulin.
 By the same token how can you permit that a molecule like gluten, for example, that’s much larger than what can come into our body, get access, and induce an immune response, unless something goes wrong in terms of gut permeability? And again, this theory has been supported by the Human Genome Project, in which some of the genes that have been discovered to be wrong with autoimmunity are genes that control gut permeability. So, I think that now this is not something that people will see as esoteric as before, so this is taking more and more ground in terms of key elements that you have to have in order to develop autoimmunity.
By the same token how can you permit that a molecule like gluten, for example, that’s much larger than what can come into our body, get access, and induce an immune response, unless something goes wrong in terms of gut permeability? And again, this theory has been supported by the Human Genome Project, in which some of the genes that have been discovered to be wrong with autoimmunity are genes that control gut permeability. So, I think that now this is not something that people will see as esoteric as before, so this is taking more and more ground in terms of key elements that you have to have in order to develop autoimmunity.
Dr. Amy Myers: So, we’ve talked a ton about leaky gut in this summit and every time, your name comes up, but I would love to hear from the man himself, your explanation of what is leaky gut.
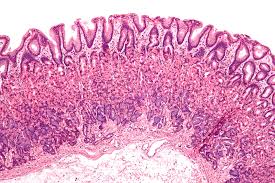 Dr. Alessio Fasano: The intestine is a very long tube. In adults, it’s roughly 20 ft. long and it’s not smooth; it has valleys and hills, and that increase the surface. If you stretch the guts of an adult on the floor, you cover a double tennis court, 3,000 sq. ft. So, until the recent past, we thought that we need that to really maximize the capability to digest and sort foodstuff, but we overlooked these other key functions, one of being communicating with the environment. This is an extremely important function; it shapes who we are because you as an individual when you were born can be considered as a marble block that is the shape, and the size, and the color is determined by your genetic makeup. But what comes out of this marble block depends on from the environment that is the sculptor that carves these blocks and whatever final product will be. Even identical twins where they were split at birth and live in two different environments, they will look very differently, meaning that the environment does a great deal in terms of determining who we are, physically or socially and in terms of activities, and so on and so forth. To do that, you need to have this continued exchange with the environment. You need to continuously have exchange of information and that exchange of molecules.
Dr. Alessio Fasano: The intestine is a very long tube. In adults, it’s roughly 20 ft. long and it’s not smooth; it has valleys and hills, and that increase the surface. If you stretch the guts of an adult on the floor, you cover a double tennis court, 3,000 sq. ft. So, until the recent past, we thought that we need that to really maximize the capability to digest and sort foodstuff, but we overlooked these other key functions, one of being communicating with the environment. This is an extremely important function; it shapes who we are because you as an individual when you were born can be considered as a marble block that is the shape, and the size, and the color is determined by your genetic makeup. But what comes out of this marble block depends on from the environment that is the sculptor that carves these blocks and whatever final product will be. Even identical twins where they were split at birth and live in two different environments, they will look very differently, meaning that the environment does a great deal in terms of determining who we are, physically or socially and in terms of activities, and so on and so forth. To do that, you need to have this continued exchange with the environment. You need to continuously have exchange of information and that exchange of molecules.
 The intestine being the largest interface with the environment is where most of this crosstalk occurs, and this long tube is covered by single-layer cells that represent this interface with the environment. One more function that again we’ve been overlooking other than to digest and sort the foodstuff is the intestine is in charge of this trafficking of molecules, not through the cell as we believed before, but in between cells. Until the recent past, the space in between cells we thought was completely sealed by sort of cement and then in the mid-80s, the Japanese groups said that’s not the case, there are doors, but they are almost always closed. Only rarely they open to allow short time to make these molecules to go back and forth, and then would be immediately closed.
The intestine being the largest interface with the environment is where most of this crosstalk occurs, and this long tube is covered by single-layer cells that represent this interface with the environment. One more function that again we’ve been overlooking other than to digest and sort the foodstuff is the intestine is in charge of this trafficking of molecules, not through the cell as we believed before, but in between cells. Until the recent past, the space in between cells we thought was completely sealed by sort of cement and then in the mid-80s, the Japanese groups said that’s not the case, there are doors, but they are almost always closed. Only rarely they open to allow short time to make these molecules to go back and forth, and then would be immediately closed.
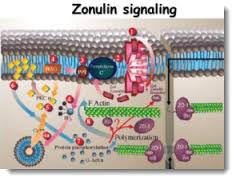 When they discovered zonulin, they discovered this could be the key of these doors if and when it’s in the picture, then we start to appreciate more and more the physiology of the mechanism. Why we do that, how this works, how we really open these doors and then we close again, and what typically happens when the physiology’s pushed to the limit, you spin into pathology. That’s when we learned that when this system is out of control, one of the most frequent conditions that you can have is indeed autoimmunity. And that’s how pretty much the field of leaky gut and its role in autoimmunity really stem into the new concept, this new mission, in which again, we have these three pillars to develop autoimmunity. Because without inappropriate antigen trafficking, that continue to bombard your body, there isn’t physically, GI-wise, a way (to develop autoimmunity)—it’s an impossible task. It’s like to pretend that you leave your room without opening the door. You need what? A way to get out or a way to get in, in this case.
When they discovered zonulin, they discovered this could be the key of these doors if and when it’s in the picture, then we start to appreciate more and more the physiology of the mechanism. Why we do that, how this works, how we really open these doors and then we close again, and what typically happens when the physiology’s pushed to the limit, you spin into pathology. That’s when we learned that when this system is out of control, one of the most frequent conditions that you can have is indeed autoimmunity. And that’s how pretty much the field of leaky gut and its role in autoimmunity really stem into the new concept, this new mission, in which again, we have these three pillars to develop autoimmunity. Because without inappropriate antigen trafficking, that continue to bombard your body, there isn’t physically, GI-wise, a way (to develop autoimmunity)—it’s an impossible task. It’s like to pretend that you leave your room without opening the door. You need what? A way to get out or a way to get in, in this case.
 Again, the reason why this (idea) has really been hard to accept, is because this completely revolutionized the concept of autoimmunity. The classical theories of antigen mimicry—you develop autoimmunity because you are exposed to microorganisms (bacteria, viruses, there are some molecules, there are structures similar but not identical to our own molecules) and the immune system that is not really focused and capable to distinguish similar but not identical molecules meant to get after this enemy and actually kills its own cells, or the bystander effect: the infection that destroy your cell’s molecules leaks out and now you attack these molecules that are your own body—would imply that once you got it, that’s it; there’s nothing you do about it. Once again, celiac disease taught us otherwise. If there’s any way that you can stop this interplay between the genes and the environment, you can eventually stop and treat autoimmunity.
Again, the reason why this (idea) has really been hard to accept, is because this completely revolutionized the concept of autoimmunity. The classical theories of antigen mimicry—you develop autoimmunity because you are exposed to microorganisms (bacteria, viruses, there are some molecules, there are structures similar but not identical to our own molecules) and the immune system that is not really focused and capable to distinguish similar but not identical molecules meant to get after this enemy and actually kills its own cells, or the bystander effect: the infection that destroy your cell’s molecules leaks out and now you attack these molecules that are your own body—would imply that once you got it, that’s it; there’s nothing you do about it. Once again, celiac disease taught us otherwise. If there’s any way that you can stop this interplay between the genes and the environment, you can eventually stop and treat autoimmunity.
 4. Datis Kharrazian, DC, DABCN, CNS: Understanding Hashimoto’s and Other Thyroid Conditions
4. Datis Kharrazian, DC, DABCN, CNS: Understanding Hashimoto’s and Other Thyroid Conditions
Dr. Amy Myers: I’m really excited about our guest today. I have Dr. Datis Kharrazian with us today, who many of you probably know if you’re suffering with thyroid disease. He’s the author of, “Why Do I Still Have Thyroid Symptoms When My Labs Are Normal?” which is an incredible book. He’s also written, “Why Isn’t My Brain Working?”  He’s a chiropractor and has a thriving practice in San Diego, helps train physicians and chiropractors around the world. In fact, I went to one of his seminars called “The Gut-Autoimmune-Gluten Connection,” and it was a fabulous seminar. I’m really excited to have him here today. Since thyroid disease is really one of the biggest subsets of autoimmunity and given your background in writing the book that you did, I thought it’d be great if we talk specifically about thyroid. Why don’t we just kind of go over autoimmune thyroid and how does that happen?
He’s a chiropractor and has a thriving practice in San Diego, helps train physicians and chiropractors around the world. In fact, I went to one of his seminars called “The Gut-Autoimmune-Gluten Connection,” and it was a fabulous seminar. I’m really excited to have him here today. Since thyroid disease is really one of the biggest subsets of autoimmunity and given your background in writing the book that you did, I thought it’d be great if we talk specifically about thyroid. Why don’t we just kind of go over autoimmune thyroid and how does that happen?
Dr. Datis Kharrazian: Well, one of the most common autoimmune diseases worldwide is autoimmune thyroid. Unfortunately, most people that have hypothyroidism never actually get diagnosed as being autoimmune because the standard of care is basically once you identify a high TSH, you’ll just be on thyroid replacement forever. The next follow-up step would be thyroid antibodies. That test is never done because it doesn’t change treatment. The treatment is still: you’re going to go back every year and then get your replacement adjusted if your TSH is up. What people tend to forget is that the model for that type of therapy is that there is an assumption that since most people that have hypothyroidism have autoimmunity, there’s no reason to test the antibodies, and that the thyroid is going to get destroyed every year more. So, every year, you need to come in and get that adjustment.
 What happens is the practitioners and insurance companies don’t really authorize or perform the thyroid antibodies, and the patient then leaves thinking they have a metabolic disease and not knowing they really have an autoimmune disease. So, thyroid antibodies really confirm that the person has an autoimmune disease. For many people, autoimmune diseases are pretty prevalent. They don’t really realize that when they have hypothyroidism, they’re actually suffering from one autoimmune disease, and it’s pretty likely that they have others and different variations of it, and things associated with autoimmunity like celiac disease or other variations. What we find is people that have hypothyroidism don’t really get their thyroid under control until they can actually address their autoimmunity.
What happens is the practitioners and insurance companies don’t really authorize or perform the thyroid antibodies, and the patient then leaves thinking they have a metabolic disease and not knowing they really have an autoimmune disease. So, thyroid antibodies really confirm that the person has an autoimmune disease. For many people, autoimmune diseases are pretty prevalent. They don’t really realize that when they have hypothyroidism, they’re actually suffering from one autoimmune disease, and it’s pretty likely that they have others and different variations of it, and things associated with autoimmunity like celiac disease or other variations. What we find is people that have hypothyroidism don’t really get their thyroid under control until they can actually address their autoimmunity.
Dr. Amy Myers: One of the biggest things of why people love your book so much is you really talk about people that go on and get (thyroid) medicine, and they’re still not getting better, or their labs are totally normal, but they’re still having a lot of these hypothyroid symptoms. So, what’s going on there when that happens?
 Dr. Datis Kharrazian: Well, there are lots of different triggers for autoimmunity, and gluten has become very popular. That’s great because we’re already used to that, but there are other foods that cross-react to gluten, and things like rice, things like corn—they can also cause the entire gluten response because they have cross-reactive responses. I really talked about that in my brain book and in my third book. The other thing that we see is simple things like blood sugar stability issues. When people have blood sugar spikes, they get IL-6 surge which stimulates the Th-17 pathway, whether they have a drop in blood sugar or have insulin surges from eating too much glucose. Those are autoimmune-promoting mechanisms, so a lot of times when we see Hashimoto’s people, it’s not just about being gluten-free or avoiding foods, it’s about stabilizing blood sugar levels.
Dr. Datis Kharrazian: Well, there are lots of different triggers for autoimmunity, and gluten has become very popular. That’s great because we’re already used to that, but there are other foods that cross-react to gluten, and things like rice, things like corn—they can also cause the entire gluten response because they have cross-reactive responses. I really talked about that in my brain book and in my third book. The other thing that we see is simple things like blood sugar stability issues. When people have blood sugar spikes, they get IL-6 surge which stimulates the Th-17 pathway, whether they have a drop in blood sugar or have insulin surges from eating too much glucose. Those are autoimmune-promoting mechanisms, so a lot of times when we see Hashimoto’s people, it’s not just about being gluten-free or avoiding foods, it’s about stabilizing blood sugar levels.
 There’s less than nutritional things you can do specifically for some of these pathways, and just recently, in the laboratory, we’ve really discovered something really profound and we’re waiting to publish it, but we’ve been checking monoclonal antibodies to TSH receptor—TSH, T4, T3, 5’deionase—and we cross-reacted with 200 different foods. So, we just got 40 new foods that we know cause molecular mimicry with thyroid, and we’re readying the manuscript to get it published. In the near future, we’re going to have a very specific autoimmune Hashimoto’s diet because we’re able to identify multiple foods that cross-react. Some cross-react with 5’deionase and now we have mechanisms for T3 conversion other than cortisol and selenium and inflammatory mechanisms, and then we’ve found specific foods that directly cross-react with T3, which would explain why some people don’t do well or don’t respond to the medications they’re taking from a molecular mimicry mechanism. So, we’re finalizing the manuscript, double-checking results, and then we’ll publish it. I think we’ll have a whole new Hashimoto’s diet beyond just gluten because many of the foods that we found are within the Paleo diet.
There’s less than nutritional things you can do specifically for some of these pathways, and just recently, in the laboratory, we’ve really discovered something really profound and we’re waiting to publish it, but we’ve been checking monoclonal antibodies to TSH receptor—TSH, T4, T3, 5’deionase—and we cross-reacted with 200 different foods. So, we just got 40 new foods that we know cause molecular mimicry with thyroid, and we’re readying the manuscript to get it published. In the near future, we’re going to have a very specific autoimmune Hashimoto’s diet because we’re able to identify multiple foods that cross-react. Some cross-react with 5’deionase and now we have mechanisms for T3 conversion other than cortisol and selenium and inflammatory mechanisms, and then we’ve found specific foods that directly cross-react with T3, which would explain why some people don’t do well or don’t respond to the medications they’re taking from a molecular mimicry mechanism. So, we’re finalizing the manuscript, double-checking results, and then we’ll publish it. I think we’ll have a whole new Hashimoto’s diet beyond just gluten because many of the foods that we found are within the Paleo diet.
Dr. Amy Myers: Many of the foods (that cross-react) are foods that people are eating on a Paleo diet?
 Dr. Datis Kharrazian: Yes. And they cross-react with the thyroid. I’m giving you one example: tuna cross-reacted, but only when it’s raw, and when it’s cooked, it doesn’t cross-react. So, the protein denatures. So, when you look at tuna, and we found some foods that are high in iodine and really cross-react with T3 and T4, but when they were cooked, there’s no cross-reactivity. We found, for example, soy didn’t cross-react unless it was processed soy. We found latex—it was one of the most devastating exposures to Hashimoto’s people—every path of the pathway: TSH, 5’deionase. These are usual things because you can package your food with latex and then you can get a reaction. You can be eating sashimi thinking it’s okay and have a cross-reactivity. These cross-reactive foods really only matter if you have antibodies against those foods. Not everyone with Hashimoto’s will, let’s say, have a reaction, but if they have, let’s say, tuna antibodies that are elevated, those tuna antibodies can cross-react with T3 due to molecular mimicry. So, some people would be very sensitive to some of those cross-reactive foods based on if they have antibodies to them, and some won’t.
Dr. Datis Kharrazian: Yes. And they cross-react with the thyroid. I’m giving you one example: tuna cross-reacted, but only when it’s raw, and when it’s cooked, it doesn’t cross-react. So, the protein denatures. So, when you look at tuna, and we found some foods that are high in iodine and really cross-react with T3 and T4, but when they were cooked, there’s no cross-reactivity. We found, for example, soy didn’t cross-react unless it was processed soy. We found latex—it was one of the most devastating exposures to Hashimoto’s people—every path of the pathway: TSH, 5’deionase. These are usual things because you can package your food with latex and then you can get a reaction. You can be eating sashimi thinking it’s okay and have a cross-reactivity. These cross-reactive foods really only matter if you have antibodies against those foods. Not everyone with Hashimoto’s will, let’s say, have a reaction, but if they have, let’s say, tuna antibodies that are elevated, those tuna antibodies can cross-react with T3 due to molecular mimicry. So, some people would be very sensitive to some of those cross-reactive foods based on if they have antibodies to them, and some won’t.
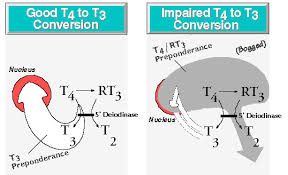 The point is that we’re doing some research now that’s really going to cause some breakthrough in our understanding, but we’ve also done monoclonal antibody testing now with various chemicals. Now, we’re getting very specific which chemicals cross-react with which part of the thyroid, and we’re now identifying certain celiac markers versus the transglutaminase 2, 3 and 6 and what part of the thyroid they impact because they impact different parts of the circuit. So, in the near future or through the next year, we will have discovered multiple mechanisms that impact conversion patterns and then receptor pathways and then the use of hormones themselves as part of being available in getting the cross-reactivity from an immune response.
The point is that we’re doing some research now that’s really going to cause some breakthrough in our understanding, but we’ve also done monoclonal antibody testing now with various chemicals. Now, we’re getting very specific which chemicals cross-react with which part of the thyroid, and we’re now identifying certain celiac markers versus the transglutaminase 2, 3 and 6 and what part of the thyroid they impact because they impact different parts of the circuit. So, in the near future or through the next year, we will have discovered multiple mechanisms that impact conversion patterns and then receptor pathways and then the use of hormones themselves as part of being available in getting the cross-reactivity from an immune response.
Dr. Amy Myers: Can you tell us about why certain people might not do well with say, Synthroid which is just T4 versus Armour’s T4 and T3 or any particular medication and how conventional medicine is typically checking only the TSH or the TSH and the free T4, not all the other components of the thyroid?
 Dr. Datis Kharrazian: Yes. When you look at the patients that suffer from thyroid disease, one of the key things is that at some point if their TSH gets tight, it’s really important for them to be on a replacement, and if they are not on replacement, they can accelerate brain degeneration and they can accelerate bone loss, they can develop gallstones. So, a lot of ugly things happen if they’re actually deficient in thyroid hormone. If someone has autoimmunity to their thyroid, at some point, the thyroid gland will be destroyed and they need to get on thyroid replacement; however, the question is, “Which type of replacement?” And you have kind of a spectrum where you have really orthodox conventional people only wanting things like levothyroxines, synthetic T4, and then we have the other side of the spectrum, we have alternative people really wanting natural bioidentical things like Nature-Throid or Armour and things like that. A lot of times, what patients get is really what the practitioner likes, and it’s not really unique to the patient and this creates some problems.
Dr. Datis Kharrazian: Yes. When you look at the patients that suffer from thyroid disease, one of the key things is that at some point if their TSH gets tight, it’s really important for them to be on a replacement, and if they are not on replacement, they can accelerate brain degeneration and they can accelerate bone loss, they can develop gallstones. So, a lot of ugly things happen if they’re actually deficient in thyroid hormone. If someone has autoimmunity to their thyroid, at some point, the thyroid gland will be destroyed and they need to get on thyroid replacement; however, the question is, “Which type of replacement?” And you have kind of a spectrum where you have really orthodox conventional people only wanting things like levothyroxines, synthetic T4, and then we have the other side of the spectrum, we have alternative people really wanting natural bioidentical things like Nature-Throid or Armour and things like that. A lot of times, what patients get is really what the practitioner likes, and it’s not really unique to the patient and this creates some problems.
 So, we found that a lot of Hashimoto’s people, for example, can’t take a bioidentical source like Armour or Nature-Throid because they can’t handle the T3 in it. We know these natural bioidenticals have some T3 in them. Some of them have such an underlying autoimmunity that as your autoimmunity destroy the thyroid gland, the tissue that’s broken down causes release of thyroid hormones and any additional T3 can make them have more anxiety and nervousness and insomnia. So, those people really don’t fall within what everyone wants them to really work which is like a bioidentical hormone with T3. Also, we have some filler issues. The filler of most of these is cornstarch, and many people that are gluten-sensitive cross-react with corn so they end up having filler issues, and there are some people that actually do better with just T4, even synthetic T4; they do better with it.
So, we found that a lot of Hashimoto’s people, for example, can’t take a bioidentical source like Armour or Nature-Throid because they can’t handle the T3 in it. We know these natural bioidenticals have some T3 in them. Some of them have such an underlying autoimmunity that as your autoimmunity destroy the thyroid gland, the tissue that’s broken down causes release of thyroid hormones and any additional T3 can make them have more anxiety and nervousness and insomnia. So, those people really don’t fall within what everyone wants them to really work which is like a bioidentical hormone with T3. Also, we have some filler issues. The filler of most of these is cornstarch, and many people that are gluten-sensitive cross-react with corn so they end up having filler issues, and there are some people that actually do better with just T4, even synthetic T4; they do better with it.
Dr. Amy Myers: So, you keep bringing up sort of this brain Hashimoto’s or brain thyroid autoimmune connection. Can you tell us more about that?
 Dr. Datis Kharrazian: Yes, I’d love to. One of the things that we see in my office, is we see most people that have Hashimoto’s have a pretty devastating decline in brain health, and part of it could be because I just love brain and I like to do brain evaluations on my patients. One paper was published in the Journal of Neurology back in 2007 and they found that thyroid antibodies can bind to cerebellar astrocytes. There is actually molecular mimicry, and recently, we found similar things in our laboratory and through our research, and what we’re finding is that many people that have thyroid antibodies, those antibodies aren’t just attacking the thyroid, but they’re also attaching to the brain; they’re attaching to the cerebellum. We also know that many people that have Hashimoto’s have gluten sensitivity, and gluten itself—gluten antibodies have been shown to cross-react with the cerebellum as well.
Dr. Datis Kharrazian: Yes, I’d love to. One of the things that we see in my office, is we see most people that have Hashimoto’s have a pretty devastating decline in brain health, and part of it could be because I just love brain and I like to do brain evaluations on my patients. One paper was published in the Journal of Neurology back in 2007 and they found that thyroid antibodies can bind to cerebellar astrocytes. There is actually molecular mimicry, and recently, we found similar things in our laboratory and through our research, and what we’re finding is that many people that have thyroid antibodies, those antibodies aren’t just attacking the thyroid, but they’re also attaching to the brain; they’re attaching to the cerebellum. We also know that many people that have Hashimoto’s have gluten sensitivity, and gluten itself—gluten antibodies have been shown to cross-react with the cerebellum as well.
 So, what we see for the most part is we see a lot of Hashimoto’s patients develop cerebellar degeneration, and what happens to them is the cerebellum starts to get degraded through this autoimmune process. They start to get balance issues, they start to get maybe occasional vertigo, trivial types of movements in their background like things flashing really upset them, they get really sensitive to light, sound, they get all these different types of neurological impairment symptoms.
So, what we see for the most part is we see a lot of Hashimoto’s patients develop cerebellar degeneration, and what happens to them is the cerebellum starts to get degraded through this autoimmune process. They start to get balance issues, they start to get maybe occasional vertigo, trivial types of movements in their background like things flashing really upset them, they get really sensitive to light, sound, they get all these different types of neurological impairment symptoms.
If it gets worse, they get ataxia, where they can’t walk straight with their eyes closed. Some of them eventually develop tremor. So, for the most part, what we’re seeing is we’re seeing a lot of thyroid patients end up with poor brain health. And here’s the thing: when the brain declines, people will get fatigue; they get brain-based fatigue, which means when they try to use their brain, they get tired, so when they try to read and they try to drive, they get tired. That’s brain-based fatigue. That’s non-metabolic fatigue; it’s using your brain with no endurance for your brain and then getting exhausted. People that have brain-based issues usually have everything blamed on their thyroid and they don’t do anything to support the brain health.  So for me, when I wrote “Why Isn’t My Brain Working?”, it’s really part two of my thyroid explanation and some people haven’t really understood that. And for most people that have thyroid dysfunction, they’re still having depression and they’re still having fatigue, especially fatigue that’s induced by using their brain. There could be a brain component to it and doing strategies just for autoimmunity and leaky gut may not be enough. You actually may need to do interventions specific for the brain. So, this is one of the things we’ve noticed. We’re trying to contribute to the knowledge base.
So for me, when I wrote “Why Isn’t My Brain Working?”, it’s really part two of my thyroid explanation and some people haven’t really understood that. And for most people that have thyroid dysfunction, they’re still having depression and they’re still having fatigue, especially fatigue that’s induced by using their brain. There could be a brain component to it and doing strategies just for autoimmunity and leaky gut may not be enough. You actually may need to do interventions specific for the brain. So, this is one of the things we’ve noticed. We’re trying to contribute to the knowledge base.
Dr. Amy Myers: And what would some of the interventions be that would be specific to the brain?
Dr. Datis Kharrazian: One of the things that I’ve done is write my book. I try to go into each mechanism and explain symptoms for each major mechanism. So, lack of oxygen to the brain is a mechanism, hypoxia of the brain is a mechanism, microglial activation is a mechanism, breach to the blood-brain barrier is a mechanism, impairments in dopamine, GABA, and acetylcholine—these are all various mechanisms. So, we go through multiple mechanisms. In the beginning of each chapter, I give lists of symptoms, and if the patient has those symptoms, that chapter’s really important for them, and then we try to get some strategies. So at the end of the day, you’re trying to see which of these mechanisms there are and really understand why a person that has a thyroid issue—if you are a thyroid patient or if you work with thyroid patients as the practitioner—why are some of these people having such severe impairments in their function? And part of this is because they’re having neurodegenerative changes. There needs to be, once the autoimmunity is somewhat managed with diet and lifestyle, an approach to really improve brain health for thyroid patients.
 5. Aristo Vojdani, PhD: Understanding Advanced Assessment and Diagnostic Tools to Track Autoimmune Disease Recovery
5. Aristo Vojdani, PhD: Understanding Advanced Assessment and Diagnostic Tools to Track Autoimmune Disease Recovery
Dr. Amy Myers: Today’s guest, I have Dr. Aristo Vojdani. I normally don’t read somebody’s bio, but I think you all maybe a little more familiar with perhaps some of the other speakers, and I don’t want you all to miss out on all the goodness of this gentleman’s background. It is amazing, so forgive me for having to read this a little bit. He is currently a professor of neuroimmunology at the Carrick Institute for Graduate Studies. Previously, he was with UCLA School of Medicine. He has a PhD in microbiology and clinical immunology, with postdoctoral studies in tumor immunology at UCLA. His research focuses on the predictive antibodies resulting in the development of numerous antibody assays.  So, a lot of people are talking about these Cyrex Labs as we’ve gone through this summit, and he is actually the chief scientific advisor, and also developing a lot of these arrays for the testing. He has 15 U.S. patents. He’s published more than 140 articles, and he’s also the CEO and technical director of Immunoscience Labs. So privileged to have you here with us. You are definitely an expert in the world of autoimmunity. So, tell me. What is autoimmunity to you?
So, a lot of people are talking about these Cyrex Labs as we’ve gone through this summit, and he is actually the chief scientific advisor, and also developing a lot of these arrays for the testing. He has 15 U.S. patents. He’s published more than 140 articles, and he’s also the CEO and technical director of Immunoscience Labs. So privileged to have you here with us. You are definitely an expert in the world of autoimmunity. So, tell me. What is autoimmunity to you?
Dr. Aristo Vojdani: Well, there is a classical definition of autoimmunity in the textbook. They tell us that autoimmunity is the process by which the immune system of an individual cannot differentiate between self and non-self, and thereby, produces antibodies against its own antigens. However, I’m going to add to that by saying that autoimmunity is a process by which the immune system of an individual, due to exposure to environmental triggers (this is the heart of the matter), cannot differentiate between self and non-self, and therefore produces antibodies against its own tissue.
Dr. Amy Myers: And what are some of these environmental triggers?
 Dr. Aristo Vojdani: Well, we have three very famous environmental triggers. Number 1, toxic chemicals or xenobiotics. Number 2, dietary components; there are many of them; and thirdly, infections. These three, plus stress, and some additional factors play a significant role in the development of autoimmunity.
Dr. Aristo Vojdani: Well, we have three very famous environmental triggers. Number 1, toxic chemicals or xenobiotics. Number 2, dietary components; there are many of them; and thirdly, infections. These three, plus stress, and some additional factors play a significant role in the development of autoimmunity.
Dr. Amy Myers: Before we get in to all that, I think you have a personal story about how you actually even got involved in autoimmunity and why that became an interest of yours? Is that true?
Dr. Aristo Vojdani: Yes, absolutely. I was about six years old when my mother had severe infection in the gut, where she was going to so-called a dental technician without having any knowledge that we should not remove any teeth. During the infection, he was removing three or four each day. And so, today, we know he exposed her to many bacterial toxins. Six years later, she started having symptoms of rheumatoid arthritis. Fifteen years later, she had full-blown rheumatoid arthritis, osteoarthritis, and then a couple of years after that, she needed total knee replacement. So, after having the knee replacement, she lived with this painful disease for additional 40-42 years of suffering with this devastating disease. During my graduate studies, I proved, indeed, her illness was initiated by toxic material released by porphyromonas gingivalis or streptococcus mutan, which is involved in oral infection.
 By looking at antibodies in her blood, she had 10 times higher levels of antibodies against these two bacterial toxins, compared to any other individual who had the same age, and they were healthy at that time. So, that was my personal interest—to look and find the causes. So therefore, today, it’s very important to talk about the causes of autoimmune disease because when we learn about the causes of autoimmune disease, we can make huge difference in preventing autoimmune diseases.
By looking at antibodies in her blood, she had 10 times higher levels of antibodies against these two bacterial toxins, compared to any other individual who had the same age, and they were healthy at that time. So, that was my personal interest—to look and find the causes. So therefore, today, it’s very important to talk about the causes of autoimmune disease because when we learn about the causes of autoimmune disease, we can make huge difference in preventing autoimmune diseases.
Dr. Amy Myers: Yes, and they are on the rise, so we definitely need to get people educated, so that they can help reverse what they have going on or prevent one from coming. So, back to what you were saying, it sounded like it was toxins, infections, and the diet, or what you’re saying the leading factors to autoimmunity. Shall we touch on each one of those individually?
 Dr. Aristo Vojdani: Yes, but let me read a couple of statements by two most prominent scientists from Johns Hopkins University if you don’t mind. I’m sure you know about the book by Donna Jackson Nakazawa, “The Autoimmune Epidemic.” Two people forwarded her book, and these are the two scientists I admire significantly. One of them is Dr. Hoke, MD, Ph.D., director of neuromuscular division of Johns Hopkins Hospital Institution, and he’s saying that:
Dr. Aristo Vojdani: Yes, but let me read a couple of statements by two most prominent scientists from Johns Hopkins University if you don’t mind. I’m sure you know about the book by Donna Jackson Nakazawa, “The Autoimmune Epidemic.” Two people forwarded her book, and these are the two scientists I admire significantly. One of them is Dr. Hoke, MD, Ph.D., director of neuromuscular division of Johns Hopkins Hospital Institution, and he’s saying that:
“It takes the human body thousands of years to adapt to new environmental stress, yet in a hundred years, we have dumped so many toxic substances into our environment that our immune system is being asked to differentiate between our own body and unrecognizable invaders nonstop, and which our body is much more likely to make a mistake than it was, say, a century ago. There are just so many opportunities to make mistakes.”
 The second professor is Dr. Noel Rose. He was the first one in the 1950s to actually demonstrate an animal model of thyroid autoimmunity. So, he’s the father of autoimmunity. And so, this is what Dr. Rose is saying:
The second professor is Dr. Noel Rose. He was the first one in the 1950s to actually demonstrate an animal model of thyroid autoimmunity. So, he’s the father of autoimmunity. And so, this is what Dr. Rose is saying:
“We have no other good explanation as to why there should be an increase in autoimmune diseases except for the things to which we are exposed in the environment. Autoimmunity is our immune system’s effort to adapt to all the new environmental agents and shifts that we are being bombarded with. It is an unsuccessful adaptation, but it is our body’s way of trying to fight back.”
 So, when so many chemicals enter the human system, it’s wrong to think that these chemicals get in and out (unchanged). Some of these chemicals get metabolized; some of these chemicals directly combine to human tissue, and therefore the immune system is going to make that mistake and cannot differentiate between self and not self, and therefore is attacking the tissue plus the chemicals, which are bound to the tissue antigens. So therefore, No. 1 importance, out of the three factors, is the chemicals—xenobiotics and toxic chemicals, and their role in autoimmunity.
So, when so many chemicals enter the human system, it’s wrong to think that these chemicals get in and out (unchanged). Some of these chemicals get metabolized; some of these chemicals directly combine to human tissue, and therefore the immune system is going to make that mistake and cannot differentiate between self and not self, and therefore is attacking the tissue plus the chemicals, which are bound to the tissue antigens. So therefore, No. 1 importance, out of the three factors, is the chemicals—xenobiotics and toxic chemicals, and their role in autoimmunity.
Dr. Amy Myers: And what can somebody do? I mean, I read that book, (The Autoimmune Epidemic by Donna Jackson Nakazawa). It’s an excellent book, and if it doesn’t make you want to race out and get a water filter or air filter and eat only organic food out of nothing plastic…but we live in the real world, so we have (I think it’s something like) 80,000 chemicals, only a fraction of which are actually being studied by the EPA to say that they’re safe, and then they’re not even testing them in combination. They’re testing them in isolation, not with the other chemicals. What can somebody do?
 Dr. Aristo Vojdani: I think education, education, education. You educate people that chemicals, most of them, are toxins. Chemicals are estrogenic compounds, that can interfere with our hormones, and so therefore, education is the most important tool that we can teach people about. For example, again, plastics—bisphenol A and many other chemicals; herbicides; pesticides. These chemicals are major contributors of autoimmunity and if we teach them, and there is a lot we can do.
Dr. Aristo Vojdani: I think education, education, education. You educate people that chemicals, most of them, are toxins. Chemicals are estrogenic compounds, that can interfere with our hormones, and so therefore, education is the most important tool that we can teach people about. For example, again, plastics—bisphenol A and many other chemicals; herbicides; pesticides. These chemicals are major contributors of autoimmunity and if we teach them, and there is a lot we can do.
 I was reading this article in Journal of Environmental Health Perspective. They took few children and they put them up on a normal diet—normal classical diet. They measured levels of the chemicals in blood and urine. It was, let’s say, 100 units. Then they changed their diet to organic food, and measured the same chemicals in blood and urine. The level dropped from 100 to almost undetectable levels. Of about, let’s say, 10 units. Five days later, they put them back on the normal diet, and chemicals went back again to 100 units. This is a classical example that indeed, we can do something about it, and organic diet can help to reduce the body load of toxic chemicals.
I was reading this article in Journal of Environmental Health Perspective. They took few children and they put them up on a normal diet—normal classical diet. They measured levels of the chemicals in blood and urine. It was, let’s say, 100 units. Then they changed their diet to organic food, and measured the same chemicals in blood and urine. The level dropped from 100 to almost undetectable levels. Of about, let’s say, 10 units. Five days later, they put them back on the normal diet, and chemicals went back again to 100 units. This is a classical example that indeed, we can do something about it, and organic diet can help to reduce the body load of toxic chemicals.
Dr. Amy Myers: I think you were credited by one of our other speakers, as saying that the Starbucks lids when you drink a hot coffee, is one of, maybe besides receipts, the biggest exposures to bisphenol A. Is that you that we need to attribute knowing that knowledge to?
 Dr. Aristo Vojdani: Yes, thank you so much. That’s one of them, but the most important one also is the sodas that we drink every day. I took the time and measured the pH of all the soda drinks. Believe me, Dr. Myers, the pH of soda is as acidic as vinegar, and so imagine, you’re putting this liquid in plastic bottles, whether it’s bisphenol A or bisphenol A-free; for me, plastic is plastic. Now, we have put that for months or years in the warehouses, supermarkets, and then we drink it. You think the pH of 2.2—that acidic like vinegar—is not going to eat up a little bit of this bisphenol A? And then we drink it every day. That’s one example.
Dr. Aristo Vojdani: Yes, thank you so much. That’s one of them, but the most important one also is the sodas that we drink every day. I took the time and measured the pH of all the soda drinks. Believe me, Dr. Myers, the pH of soda is as acidic as vinegar, and so imagine, you’re putting this liquid in plastic bottles, whether it’s bisphenol A or bisphenol A-free; for me, plastic is plastic. Now, we have put that for months or years in the warehouses, supermarkets, and then we drink it. You think the pH of 2.2—that acidic like vinegar—is not going to eat up a little bit of this bisphenol A? And then we drink it every day. That’s one example.
A second example which also is bothering me a lot is aluminum. An article published in a journal called Mucosal Immunology three months ago, showed in animal models, by introducing aluminum, it could induce an IBD (inflammatory bowel disease)-like syndrome, and then they wanted to find what is the mechanism of action because before that, we knew that aluminum accumulated in the muscle and in the brain, that’s why the connection with Alzheimer’s disease. 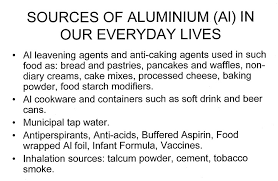 This time, they found actually about 40-60% of aluminum get into the epithelial cells, which are the protective layer of the GI tract. And so, therefore, here we are talking so much about gluten, we are talking about so much dairy product – their proteins—but how many people know that aluminum is as toxic to some individual as gluten or other dietary protein. Also, unfortunately, when they stopped putting mercury in the vaccines, now, aluminum is used as an adjuvant. An adjuvant is a material which can enhance the immune system, in this case, to produce more antibodies, but as you know, that when the body makes more antibodies, it can make more mistakes also. And possibly, autoimmunity down the road.
This time, they found actually about 40-60% of aluminum get into the epithelial cells, which are the protective layer of the GI tract. And so, therefore, here we are talking so much about gluten, we are talking about so much dairy product – their proteins—but how many people know that aluminum is as toxic to some individual as gluten or other dietary protein. Also, unfortunately, when they stopped putting mercury in the vaccines, now, aluminum is used as an adjuvant. An adjuvant is a material which can enhance the immune system, in this case, to produce more antibodies, but as you know, that when the body makes more antibodies, it can make more mistakes also. And possibly, autoimmunity down the road.
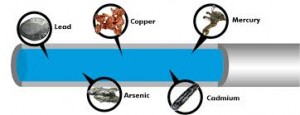 There are many other heavy metals. Lots of toxic chemicals are contributing to environmentally induced autoimmunity. In fact, I did share with you one of my articles from Journal of Autoimmune Disease. That special issue of the journal was put together by myself as the editor-in-chief of that issue only. I highly recommend it for those who are interested. They can download and read this article. My particular article is about the potential link between environmental triggers and autoimmunity, and for each environmental trigger, I’m giving the mechanism of action. So when we learn about mechanism of action, then we can also plan some kind of strategies to prevent autoimmune diseases. Number one are the toxic chemicals.
There are many other heavy metals. Lots of toxic chemicals are contributing to environmentally induced autoimmunity. In fact, I did share with you one of my articles from Journal of Autoimmune Disease. That special issue of the journal was put together by myself as the editor-in-chief of that issue only. I highly recommend it for those who are interested. They can download and read this article. My particular article is about the potential link between environmental triggers and autoimmunity, and for each environmental trigger, I’m giving the mechanism of action. So when we learn about mechanism of action, then we can also plan some kind of strategies to prevent autoimmune diseases. Number one are the toxic chemicals.
If I were to give you a statistic based on my own personal experience from working in the lab for more than 40 years, and in clinical immunology level more than 30 years, and handling blood samples of patients exposed to toxic chemicals, I would say, out of the three factors, the most important one that are contributing to autoimmune diseases are toxic chemicals in about 50-60% of the cases, dietary components in about 30-40% of the cases; and infections in only about 10% of the cases.
Dr. Amy Myers: Cyrex has a new array, Array 11, that looks at antibodies to certain toxins. Is that correct?
 Dr. Aristo Vojdani: Yes, correct, and those who are interested to read the science behind this array, Array 11, which are measuring IgG and IgA antibodies against 12 most common chemicals including heavy metals and bisphenol A, fire retardants, formaldehyde, and so forth, they can read my recent article, which was published this week in the Journal of Applied Toxicology. The title of this article is “Elevated Levels of Antibodies Against Xenobiotics in a Subgroup of Healthy Subject.” Why was I interested in healthy subjects? Because all of us are exposed to toxic chemicals on daily basis. I wanted to see what is the percentage of population, which chemicals bind to their tissue and results in antibody production against, for example, human serum albumin, which is the most prominent protein in the blood, plus some of these chemicals. And we found about 20-25% of the healthy population make antibodies against their own tissue antigens plus these toxic chemicals. So, if it continues like this, these individuals, in my opinion, will be more prone to autoimmune diseases in the future.
Dr. Aristo Vojdani: Yes, correct, and those who are interested to read the science behind this array, Array 11, which are measuring IgG and IgA antibodies against 12 most common chemicals including heavy metals and bisphenol A, fire retardants, formaldehyde, and so forth, they can read my recent article, which was published this week in the Journal of Applied Toxicology. The title of this article is “Elevated Levels of Antibodies Against Xenobiotics in a Subgroup of Healthy Subject.” Why was I interested in healthy subjects? Because all of us are exposed to toxic chemicals on daily basis. I wanted to see what is the percentage of population, which chemicals bind to their tissue and results in antibody production against, for example, human serum albumin, which is the most prominent protein in the blood, plus some of these chemicals. And we found about 20-25% of the healthy population make antibodies against their own tissue antigens plus these toxic chemicals. So, if it continues like this, these individuals, in my opinion, will be more prone to autoimmune diseases in the future.
 So, it is highly important to test for antibodies against these chemicals, and based on this, to implement some kind of programs to eliminate these chemicals from the environment of those patients, even if they do not yet have autoimmune disease. They may be in the process of developing autoimmune disease—maybe they have autoimmune reactivity. Additionally, testing for Array 5, which is measuring antibodies against 24 different tissue antigens to different organ tissues (can be very useful).
So, it is highly important to test for antibodies against these chemicals, and based on this, to implement some kind of programs to eliminate these chemicals from the environment of those patients, even if they do not yet have autoimmune disease. They may be in the process of developing autoimmune disease—maybe they have autoimmune reactivity. Additionally, testing for Array 5, which is measuring antibodies against 24 different tissue antigens to different organ tissues (can be very useful).