 NSAID-Induced Enteropathy
NSAID-Induced Enteropathy
NSAID-induced enteropathy refers to intestinal damage that occurs from the use of non-steroidal anti-inflammatory drugs (NSAIDs). Examples of NSAIDs include ibuprofen (Advil®, Motrin®), naproxen (Aleve®, Naprosyn), Celebrex® and aspirin. The use of NSAIDs, including aspirin, is common in the treatment of pain, inflammation, and fever. Additionally, low-dose aspirin is used routinely in the prevention of heart attack and stroke. These drugs, both through prescription and over-the-counter (OTC) use, are the most widely used class of medications in the United States.[352] Not surprisingly, NSAID use increases among the elderly. In a survey of people 65 years of age and older, 70% used NSAIDs at least once weekly, and 34% used them at least daily! The prevalence of at least weekly aspirin usage was 60%![353] More than 111 million NSAID prescriptions were written in 2004.[354]
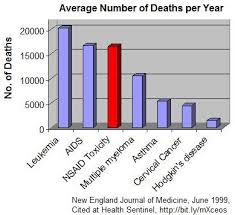 Much of this usage comes from pain conditions, such as arthritis and related musculoskeletal complaints. In 1990, the estimated prevalence of self-reported arthritis in the U.S. was 37.9 million cases, or 15% of the population! By 2020, it is projected that 59.4 million will be affected—a 57% increase from 1990![355] As the incidence of arthritis complaints increases, the use of prescription and OTC NSAIDs is also expected to increase.[356] However, the use of NSAIDs does not come without risks. The most common risk of NSAID use is damage to the stomach (gastropathy) and intestinal lining (enteropathy). Iron-deficient anemia is a common first sign of NSAID-enteropathy (due to internal bleeding), and serious complications can include massive bleeding, perforation and strictures, sometimes leading to death.[357]
Much of this usage comes from pain conditions, such as arthritis and related musculoskeletal complaints. In 1990, the estimated prevalence of self-reported arthritis in the U.S. was 37.9 million cases, or 15% of the population! By 2020, it is projected that 59.4 million will be affected—a 57% increase from 1990![355] As the incidence of arthritis complaints increases, the use of prescription and OTC NSAIDs is also expected to increase.[356] However, the use of NSAIDs does not come without risks. The most common risk of NSAID use is damage to the stomach (gastropathy) and intestinal lining (enteropathy). Iron-deficient anemia is a common first sign of NSAID-enteropathy (due to internal bleeding), and serious complications can include massive bleeding, perforation and strictures, sometimes leading to death.[357]
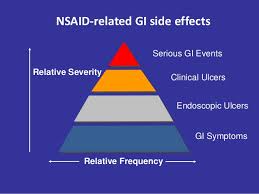 “The prevalence and clinical significance of NSAID-enteropathy continues to be greatly under-recognized. NSAID-induced enteropathy and bleeding occur more frequently than NSAID induced gastropathy. Significant small intestinal damage and bleeding can be observed in about 70% of chronic NSAID users, and in the majority of patients the injury is sub-clinical.”[357]
“The prevalence and clinical significance of NSAID-enteropathy continues to be greatly under-recognized. NSAID-induced enteropathy and bleeding occur more frequently than NSAID induced gastropathy. Significant small intestinal damage and bleeding can be observed in about 70% of chronic NSAID users, and in the majority of patients the injury is sub-clinical.”[357]
Wow! Significant damage to the small damage occurs in 70% of chronic NSAID users! This information should be more widely publicized! These medications should be clearly labeled and doctors should be warning their patients about the risks associated with these drugs with every prescription. On top of that, in most cases the injury is subclinical (meaning it does not cause any symptoms or signs)!  If the injury is subclinical, it can’t be very serious, right? Unfortunately, that’s not the case.
If the injury is subclinical, it can’t be very serious, right? Unfortunately, that’s not the case.
“…even minor and subclinical injury to the intestinal mucosa can result in significant, though delayed, metabolic consequences, which may seriously affect the health of an individual.” [358]
“With improvements in the detection of NSAID-induced damage in the small intestine, it is now clear that this injury and the associated bleeding occurs more frequently than that occurring in the stomach and duodenum, and can also be regarded as more dangerous.”[357]
 It is common practice in primary care and pain management to prescribe acid-suppressing medications (PPIs such as omeprazole) together with NSAIDs in order to protect the intestinal tract and reduce risk of GI adverse effects. However, recent research indicates that this can worsen the damage to the GI tract.
It is common practice in primary care and pain management to prescribe acid-suppressing medications (PPIs such as omeprazole) together with NSAIDs in order to protect the intestinal tract and reduce risk of GI adverse effects. However, recent research indicates that this can worsen the damage to the GI tract.
“Moreover, recent studies suggest that commonly used drugs for protecting the upper gastrointestinal tract (i.e., proton pump inhibitors) can significantly worsen NSAID-induced damage in the small intestine.”[357]
“The frequent use of PPIs can exacerbate NSAID-induced small intestinal injury by altering intestinal microbiota. Thus, the use of PPI is considered to be an independent risk factor associated with NSAID-associated enteropathy.”[358]
 Mechanism of Injury of NSAIDs to Gut Lining
Mechanism of Injury of NSAIDs to Gut Lining
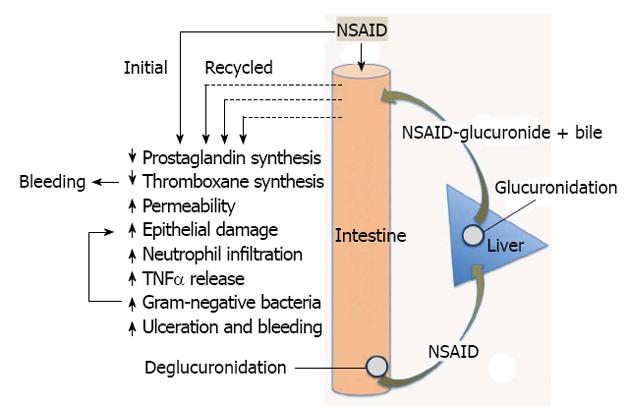
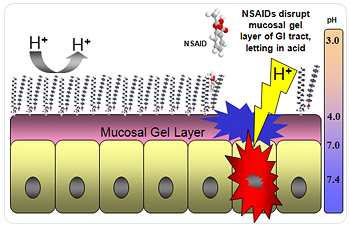
How do NSAIDs cause damage to the gut? Let’s take a more in-depth look at how NSAIDs injure the gut lining. This may be a bit technical for some readers but others will find this informative. NSAIDs cause topical injury to the mucosal lining of the GI tract and systemic effects (throughout the body) by inhibiting the COX enzymes resulting in prostaglandin depletion. COX (cyclooxygenase) is an enzyme that is responsible for the production of prostaglandins and thromboxane. Prostaglandins are lipid compounds that have a wide range of hormone-like effects in the body. Tissue prostaglandins are produced via two distinct enzyme-dependent pathways: a COX-1 and a COX-2 pathway.
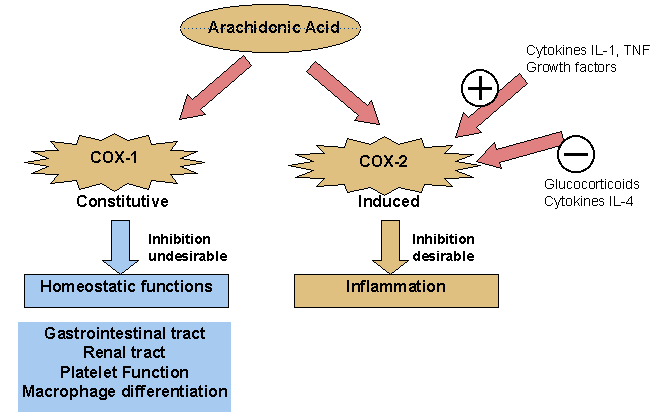 The COX-1 pathway is the predominant constitutive (replenishing) pathway; prostaglandins derived from this enzyme mediate many effects, most notably aiding in gastroduodenal protection, renal perfusion, and platelet activity. The COX-2 pathway, in contrast, is inducible by inflammatory stimuli and primarily mediates effects through prostaglandins which result in inflammation, pain, and fever. NSAIDs work by blocking these two important enzymes throughout the body. Inhibition of the COX-1 pathway blocks production of prostaglandins that play an important protective role in the stomach by increasing mucosal blood flow, stimulating the synthesis and secretion of mucus critical for the mucosal lining, and promoting proliferation of the epithelial lining. Secretion of mucus and epithelial proliferation are critical aspects to gut health in order to prevent intestinal permeability or leaky gut!
The COX-1 pathway is the predominant constitutive (replenishing) pathway; prostaglandins derived from this enzyme mediate many effects, most notably aiding in gastroduodenal protection, renal perfusion, and platelet activity. The COX-2 pathway, in contrast, is inducible by inflammatory stimuli and primarily mediates effects through prostaglandins which result in inflammation, pain, and fever. NSAIDs work by blocking these two important enzymes throughout the body. Inhibition of the COX-1 pathway blocks production of prostaglandins that play an important protective role in the stomach by increasing mucosal blood flow, stimulating the synthesis and secretion of mucus critical for the mucosal lining, and promoting proliferation of the epithelial lining. Secretion of mucus and epithelial proliferation are critical aspects to gut health in order to prevent intestinal permeability or leaky gut!
 The inhibition of these prostaglandins by NSAIDs impairs these protective factors, resulting in a gastric lining that is more susceptible to acid, pepsin, and bile salts and more permeable to toxic intestinal compounds (affect intestinal permeability). A major consequence of prostaglandin depletion is to create an environment that is conducive to peptic ulcer formation, bleeding and serious GI complications. Since prostaglandins are essential to both the maintenance of intact GI defenses and normal platelet function, NSAIDs, including aspirin, promote ulcer formation as well as bleeding.[356] This is why NSAIDs are also considered a major risk factor for intestinal permeability.
The inhibition of these prostaglandins by NSAIDs impairs these protective factors, resulting in a gastric lining that is more susceptible to acid, pepsin, and bile salts and more permeable to toxic intestinal compounds (affect intestinal permeability). A major consequence of prostaglandin depletion is to create an environment that is conducive to peptic ulcer formation, bleeding and serious GI complications. Since prostaglandins are essential to both the maintenance of intact GI defenses and normal platelet function, NSAIDs, including aspirin, promote ulcer formation as well as bleeding.[356] This is why NSAIDs are also considered a major risk factor for intestinal permeability.
 Selective COX-2 Inhibitors
Selective COX-2 Inhibitors
What about the newer class of NSAIDs, known as the selective COX-2 inhibitors or “coxibs”, such as Celebrex®? Aren’t they safer for the gut than the other NSAIDS? In the 1990’s, a tremendous amount of research was focused on understanding the physiology and pharmacology of these two distinct COX enzymes, largely fueled by the interest of several large pharmaceutical companies in the notion that selective inhibitors of COX-2 would provide all of the anti-inflammatory activities of NSAIDs without the major adverse effects on the GI lining.[357]
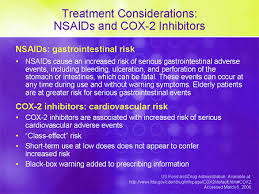 “However, as the science of COX-2 caught up with the marketing of COX-2, it became evident that the delineation of functions of the two COX enzymes was not so clear-cut as had been proposed and heavily promoted. COX-1 contributes significantly to inflammation while COX-2 contributes significantly to many physiological functions, including mucosal defense.”[357]
“However, as the science of COX-2 caught up with the marketing of COX-2, it became evident that the delineation of functions of the two COX enzymes was not so clear-cut as had been proposed and heavily promoted. COX-1 contributes significantly to inflammation while COX-2 contributes significantly to many physiological functions, including mucosal defense.”[357]
So we now know that these selective COX-2 inhibitor medications, which were touted as safe for the stomach and GI tract by the pharmaceutical companies, are not safe for the gut either.
 Conventional Management of NSAID-Induced Enteropathy
Conventional Management of NSAID-Induced Enteropathy
There is no known drug treatment for NSAID-induced enteropathy, other than the withdrawal of use of NSAIDs. Some doctors may still recommend the use of PPIs in these cases, however, as we have seen, recent literature has shown that the use of PPIs increases intestinal damage, rather than alleviates it.
“Moreover, recent studies suggest that commonly used drugs for protecting the upper gastrointestinal tract (i.e., proton pump inhibitors) can significantly worsen NSAID-induced damage in the small intestine.”[357]
 Clinical Management of NSAID-Induced Enteropathy in Functional Medicine
Clinical Management of NSAID-Induced Enteropathy in Functional Medicine
As we have seen from the previous section on natural compounds used in the treatment of intestinal permeability, various plant compounds, vitamins and minerals have been shown in the literature to have a restorative effect on a damaged intestinal lining.[288-351] Many of the compounds that are used to treat intestinal permeability or gastric and duodenal ulcers are also used to in the treatment for NSAID-induced enteropathy. The reason for this is because these compounds have a restorative effect on the mucosal epithelial lining of the GI tract. In other words, they help the GI tract regenerate healthy epithelial cells which make up the GI lining.
 As you may have noticed, in addition to NSAID-induced enteropathy, NSAIDs are a risk factor for both gastric and duodenal ulcers and intestinal permeability. This is because NSAIDs cause damage to the epithelial lining that lead to all of these conditions which are closely related. They are all mediated by damage to this epithelial lining. In fact, one of the methods used to study the effects of drug or plant compounds on a damaged gastric or intestinal mucosal lining is to give rats high-dose NSAIDs to induce this mucosal damage.[293-295,299] In addition to these plant compounds used for the treatment of damage to the gastric and intestinal lining, the omega-3 polyunsaturated fatty acids (n-3 PUFAs) found in
As you may have noticed, in addition to NSAID-induced enteropathy, NSAIDs are a risk factor for both gastric and duodenal ulcers and intestinal permeability. This is because NSAIDs cause damage to the epithelial lining that lead to all of these conditions which are closely related. They are all mediated by damage to this epithelial lining. In fact, one of the methods used to study the effects of drug or plant compounds on a damaged gastric or intestinal mucosal lining is to give rats high-dose NSAIDs to induce this mucosal damage.[293-295,299] In addition to these plant compounds used for the treatment of damage to the gastric and intestinal lining, the omega-3 polyunsaturated fatty acids (n-3 PUFAs) found in  fish oils (EPA and DHA) have been found to have a significant protective effect on the GI lining against NSAID-induced GI damage.[359] In fact, a large gastroenterology medical journal just recently published an article claiming that, due to the protective effects of these fatty acids, the next generation of NSAIDs will include these omega-3 fatty acids in the drug.
fish oils (EPA and DHA) have been found to have a significant protective effect on the GI lining against NSAID-induced GI damage.[359] In fact, a large gastroenterology medical journal just recently published an article claiming that, due to the protective effects of these fatty acids, the next generation of NSAIDs will include these omega-3 fatty acids in the drug.
“Because n-3 PUFAs have been proven to attenuate cytotoxicity, inhibit lipid-raft-associated harmful signaling, and relieve oxidative stress relevant to NSAIDs, n-3 PUFA based NSAIDs will be next-generation GI-safe NSAIDs.”[359]
Related Articles
Hypochlorhydria (Low Stomach Acid)
Gastroesophageal Reflux Disease (GERD)
Intestinal Permeability/Leaky Gut
Irritable Bowel Syndrome (IBS)
Small Intestinal Bacterial Overgrowth
The Neuroendocrine System of the Gut and the Brain-Gut Axis
References
352. Abraham N.S., El-Serag H.B., Johnson M.L.; National adherence to evidence-based guidelines for the prescription of nonsteroidal anti-inflammatory drugs. Gastroenterology. 129 2005:1171-1178.
353. Talley N.J., Evans J.M., Fleming K.C., Harmsen W.S., Zinsmeister A.R., Melton L.J. III; Nonsteroidal antiinflammatory drugs and dyspepsia in the elderly. Dig Dis Sci. 40 1995:1345-1350.
354. Shaheen N.J., Hansen R.A., Morgan D.R.; The burden of gastrointestinal and liver diseases, 2006. Am J Gastroenterol. 101 2006:2128-2138.
355. Lawrence R.C., Helmick C.G., Arnett F.C.; Estimates of the prevalence of arthritis and selected musculoskeletal disorders in the United States. Arthritis Rheum. 41 1998:778-799.
356. Deepak L. Bhatt, et al. ACCF/ACG/AHA 2008 Expert Consensus Document on Reducing the Gastrointestinal Risks of Antiplatelet Therapy and NSAID Use. A Report of the American College of Cardiology Foundation Task Force on Clinical Expert Consensus Documents. J Am Coll Cardiol. 2008;52(18):1502-1517. doi:10.1016/j.jacc.2008.08.002
357. John L Wallace. Mechanisms, prevention and clinical implications of nonsteroidal anti-inflammatory drug-enteropathy. World J Gastroenterol. 2013 March 28; 19(12): 1861–1876. Published online 2013 March 28. doi: 10.3748/wjg.v19.i12.1861
358. Marlicz W1, Loniewski I2, Grimes DS3, Quigley EM4. Nonsteroidal anti-inflammatory drugs, proton pump inhibitors, and gastrointestinal injury: contrasting interactions in the stomach and small intestine. Mayo Clin Proc. 2014 Dec;89(12):1699-709. doi: 10.1016/j.mayocp.2014.07.015. Epub 2014 Oct 29.
359. Park JM1, Han YM, Jeong M, Kim EH, Ko WJ, Cho JY, Hahm KB. Omega-3 polyunsaturated fatty acids as an angelus custos to rescue patients from NSAID-induced gastroduodenal damage. J Gastroenterol. 2015 Jan 13. [Epub ahead of print]